Atypical HUS: A Fragmented Landscape
Breaking Down Clinical Trial Challenges
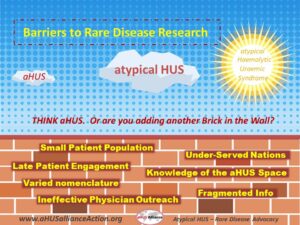
Research advancements and therapeutic drug development hold common challenges, which are heightened in the rare disease space for ultra-rare conditions as atypical HUS. News and research related to atypical hemolytic uremic syndrome, or aHUS, may be grouped under diverse headings such as ‘thrombotic microangiopathy’ or ‘complement dysregulation’ as well as variants in spelling of the disease name or differences in terminology (e.g. complement-mediated TMA or CM-TMA). Fragmented information flow in the aHUS arena has lead to creation of additional barriers for all stakeholders, to include patients, physicians, advocacy groups, research teams, communication firms, pharmaceutical companies, and those involved in development of clinical trials.
In Spring 2018 the aHUS Alliance website featured a four-part series on common misperceptions held regarding rare disease advocacy, which explored several key facets related to this clinical trials, including Pathways of Patient Engagement & Recruitment. Are people exercising due diligence to determine the needs and key issues in the aHUS space prior to launching initiatives? Factors in clinical trials within the aHUS space, and issues important to those who seek to develop new therapeutic drugs, have been noted across national and international aHUS social media and websites. Case in point, our aHUS Alliance May 2018 drug discovery and market factors overview which detailed specific issues seen as barriers to aHUS clinical trials.
Despite the 3rd aHUS Awareness Day, founded by the aHUS Alliance in 2015 and marked each 24 September, there continues to be a lack of connectivity among information and interests within and throughout the atypical HUS arena. Why? Professional journals and conferences outline current aHUS research and point out gaps in its knowledge base. Physicians around the world are concerned about lack of drug access and indicate desire for both more physician education and for expanded treatment options, as evidenced by the 2018 proposal for a Global Review Panel for aHUS Drug Access. With advocates from many nations, the aHUS Alliance believes that each nation’s atypical HUS advocacy group can offer insights relative to the differing government and healthcare policies. (Click HERE for the list of national aHUS advocacy outlets). There are core issues which affect multiple countries and go beyond borders, and it is these which the aHUS Alliance addresses through its efforts and actions. Our group’s background information continually grows and updates as we connect with aHUS research teams, most recently through the aHUS Alliance EU whistle-stop tour in July 2018 with visits to 4 centres in three nations. Great work is being done in the field of atypical HUS research, and growth of its knowledge base.
It’s troubling that readily available information about needs, concerns, insights and networking related to atypical HUS currently remain under-utilized by stakeholders prior to their launch of initiatives in this arena. There’s a disconnect when the aHUS Alliance hears from its network of aHUS investigators and clinicians that they have keen interest in expanded treatment options, while clinical trial leaders note difficulty in recruiting physicians interested in new therapeutic drugs. Efforts in the aHUS arena arguably could be more effective and efficient by targeting key aspects frequently noted by the aHUS Alliance: early and correct diagnosis of atypical HUS (differentiating medical conditions with similar presentations), inclusion and recognition of varied aHUS clinical subtypes within patient engagement efforts, focus on underserved nations without current access to eculizumab, noting drug delivery system ease and drug price point for new therapeutics, and targeting outreach and education efforts.The aHUS Alliance has continued to express needs and opportunities, outlining these areas repeatedly across multiple articles and initiatives.
People and companies used to working with other rare disease populations may find their years of background don’t necessarily translate well within the atypical HUS arena. Depth of background and awareness of current disconnects within this competitive landscape should be integral to a proactive approach for stakeholders. As volunteers who are either adult aHUS patients or family caregivers, rather than professionals or paid staff, the aHUS Alliance global action team has assisted physicians with outreach for conferences (SEPTWG/IPNA in Bucharest) and has been integral in certain highly-targeted physician education efforts (such as TMA Boston). We’re aware how general issues such as those below can cause barriers for those interested in aHUS drug discovery, clinical trials, and other areas:
- Atypical HUS: Often delayed & difficult diagnosis, some lack of consensus among experts.
- Proactive Approach: Need for stakeholder inclusion prior to launching initiatives
- Multiple Disciplines: Outreach based on recognition that aHUS patients are seen by varied specialists
- Communication Flow: Currently fragmented on most websites and press releases, compounded by multiple variants of terminology and key words (also an issue for journals & at conferences)
- Utilizing Current Assets & Info: Little awareness of key issues in the global aHUS community, from physicians and advocates
As an aHUS advocacy organization, the aHUS Alliance is dedicated to connecting people, information, and efforts that serve to grow opportunities and advancements that promote better patient outcomes. In that spirit, we outline considerations which may in part address and mitigate current barriers to atypical HUS clinical trial development, outreach, and recruitment efforts. Could re-thinking current barriers act to target opportunities and provide the momentum needed to positively impact clinical trial enrollment?
Take A Fresh Look at Areas for
Outreach & Recruitment in aHUS Arena
Intensivists & Critical Care settings
Diagnosis of patients with atypical HUS is challenging since aHUS is largely a diagnosis of exclusion. There’s no simple and definite test to diagnose this very rare and life-threatening disease, which often presents with characteristics of more common medical conditions. Differentiating among forms of thrombotic microangiopathy has figured in multiple medical journals and among conference topics for both nephrology and hematology, and therefore was highlighted in aHUS Alliance information and efforts over the past two years. Recently, we’ve noticed a new trend.
Over the past few months, there have been 3 publications centered on distinguishing among forms of TMA in critical care settings, with one specific to atypical HUS (see list below). If diagnosis of new cases of aHUS take place in the ICU, is this aspect an uncaptured opportunity regarding aHUS diagnosis, regarding enrollment of new and naive-treatment patients? Education and outreach to intensivists and others in critical care settings may serve as a new pathway with potential regarding aHUS outreach and recruitment regarding research and clinical trials.
aHUS & TMA in Critical Care:
Recent publications regarding Differentiation, Diagnosis, Treatment
- Azoulay E et al. Expert Statements on the Standard of Care in Critically Ill Adult Patients With AtypicalHemolytic Uremic Syndrome. CHEST Journal, Vol 152, Issue 2 , 424 – 434. Aug 2017
- Rafat J et al. Early Differentiation of Shiga Toxin-Associated Hemolytic Uremic Syndrome in Critically Ill Adults With Thrombotic Microangiopathy Syndromes. Crit Care Med. 2018 Sep;46(9):e904-e911
- Vincent JL et al. Thrombocytopenia in the ICU: disseminated intravascular coagulation and thromboticmicroangiopathies—what intensivists need to know. Crit Care. 2018; 22: 158. 13 June 2018
Obstetrics: More to Consider
At the aHUS Alliance we sometimes ponder, “We recognize this as an area of concern, so why aren’t others?” and frankly, we remain perplexed. Pregnancy and atypical HUS has been a key topic of interest and research over recent years. Researchers and clinicians have addressed aHUS and pregnancy, to include journal articles and YouTube videos of clinical presentations. Given this, wouldn’t it make sense to reach out to the ob/gyn community to open an ongoing dialogue about differentiating pre-eclampsia and HELLP from atypical HUS and other syndromes of thrombotic microangiopathy?
Awareness of pre-eclampsia certainly exists. Pregnant women often hear about monitoring blood pressure as way to watch for possible pre-eclampsia as a pregnancy complication (which in severe cases may impair kidney or liver function) and in 1982 obstetricians became aware of a related subset of clinical conditions termed HELLP syndrome (involving Hemolysis, ELevated liver enzymes, and Low Platelet count). If a patient presents with this triad of symptoms, which also occur with atypical HUS, physicians must delve deeper to determine the root cause.
“Due to overlapping clinical and laboratory features, TTP and aHUS are often mistaken for preeclampsia or HELLP. Unfortunately, delays in appropriate diagnosis and treatment may be life-threatening. Our objective is to alert obstetrician-gynecologists, certified nurse midwives, family medicine providers, and subspecialty consultants, to the range of TMA disorders that may occur in and around pregnancy.” Thrombotic microangiopathies of pregnancy: Differential diagnosis. (Gupta M et al, 2018)
A patient’s history of atypical HUS activity may exist prior to pregnancy, but pregnancy can trigger a patient’s initial presentation with aHUS. There’s an existing body of excellent work done on the topic pregnancy and TMAs, some specific to atypical HUS, which include variants in trimester timing versus postpartum events and which along with ADAMTS13 testing may help differentiate conditions and aid diagnosis. Since researchers as well as aHUS advocacy groups have targeted pregnancy as an important topic, shouldn’t the field of obstetrics be considered as a viable option to explore regarding outreach, education, and clinical trial recruitment?
For more on ‘aHUS & Pregnancy’, see the Research & Publications Section of our Info Center
ADAMTS13 Testing: A Springboard?
Since the advent of the complement inhibitor eculizumab, more emphasis has been placed on accurate and rapid diagnosis of atypical HUS and its differentiation from TTP (thrombotic thrombocytopenic purpura) and other forms of thrombotic microangiopathy. Symptoms and lab results, together with ADAMTS13 testing, can provide vital information to craft appropriate patient treatment plans although ADAMTS13 values alone do not establish or exclude certain diagnoses.
“Rapid differential diagnosis is needed in order to determine the specific type of thrombotic microangiopathy that is present, because only patients with TTP and only a very small percentage of those with atypical hemolytic-uremic syndrome (aHUS) can benefit from plasmapheresis.” The Differential Diagnosis and Treatment of Thrombotic Microangiopathies (Bommer et al, 2018)
“Diagnosis can be difficult, as there is clinical overlap with haemolytic uraemic syndrome (HUS), autoimmune disease and a spectrum of pregnancy‐related problems.” Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies (Scully et al, 2012)
References to the value of ADAMTS13 testing at initial presentation abound during reviews of the literature regarding diagnosis of atypical HUS, to include challenges with differentiating it from other medical conditions with similar clinical characteristics. But what happens next, after clinicians have the results of ADAMTS13 and lab results, and their initial suspicions of atypical HUS are supported by quantitative date? How do patient care plans get crafted, and how might clinicians get informed with an expedited and accurate overview about new clinical trials?
Availability of ADAMTS13 testing is broad and varied in scope. Some hospitals are well equipped with in-house laboratories, while others outsource ADAMTS13 testing to regional labs or large corporate diagnostic service platforms. ADAMTS13 screening may be done within platforms offering a unified approach, which may improve patient outcomes by interpreting lab results as part of a holistic and informed approach to personalized patient care plans. Research, clinical, and academic efforts often form a collaborative and multidisciplinary approach at aHUS and TMA study centers, which can include ADAMTS13 testing among early diagnostic tools before moving along to detailed genetic screening. In Atypical Hemolytic Uremic Syndrome: A Brief Review (Zhang K et al, 2017), Table 2 notes some of the companies and groups which make available ‘Commercially available diagnostic atypical hemolytic uremic syndrome test panels’.
Could ADAMTS13 testing pre-identify possible aHUS patients, creating a potential pool of newly diagnosed individuals for who could benefit from clinical trials? Yes, although we must underscore patient privacy and other varied concerns of an ethical or commercial nature, to include the regulatory environments as well as aspects of scientific methodology. It’s challenging to juggle such an array of considerations to maintain ethical balance with the responsibility of healthcare providers to provide information and treatment options. ADAMTS13 as a portal for patient recruitment is an interesting and largely untapped topic for clinical trial leads within pharma whose drug discovery pipelines show potential for therapeutics of interest to the atypical HUS community (Table 1, overview Atypical HUS: 2018 Therapeutic Drug Discovery). Given the amount of competition for those offering ADAMTS13 testing, and the financial incentives for complement inhibitors and other drugs in this niche space, what are companies doing to reach out various groups (regarding critical care, obstetrics, ADAMTS13 testing) for TMA and aHUS ‘Med Ed’? And what collaborative opportunities may exist to forge an innovative path to move forward clinical trials?
For more on ‘aHUS Diagnosis’ and ‘aHUS as a Thrombotic Microangiopathy’, see the Research & Publications Section of our Info Center
Stakeholders: Early & Informed Contact
There’s a current disconnect among stakeholders in the aHUS arena. Physicians and patient advocates are voicing clear needs for a more robust information stream regarding patient care plans and desire for expanded clinical trials. How then can communication firms, corporate interests, market survey teams, and clinical trial leaders note limited interest or engagement when patients and their physicians repeatedly raise their voices about the needs within the aHUS community? Who’s listening, and to what?
Contact is often made after projects have been fully framed, surveys created, and initiatives launched. Why are aHUS patients, and the physicians who treat them, provided so few opportunities at initial stages of research and drug discovery? With any product coming to the marketplace, a wide net is usually cast to determine essential factors likely to determine commercial success of innovations that aim to be safe, effective, and at a reasonable price point given market factors. Focus groups are usually tapped for initial input and throughout the process, to refine and retool as needed. This should hold true as well for orphan drug development – and perhaps even more so.
Any drug for a rare disease like atypical HUS needs to consider price and drug access concerns – and these are not unrelated matters. Rare disease policies vary from country to country, and many government healthcare systems consider price point as a critical tipping point to maintain their financial bottom lines for national health services and approved treatment options. How well do physicians and patients understand the process of bringing a new drug to market, phases of clinical trials, selection of clinical trial locations, and the important roles they can play at each step?
“Health care professionals, regulators, communication media, patient associations, and pharmaceutical companies need to collaborate to provide proper information about the purposes of research and the mechanisms available to protect participants. Society must realize that there is no progress without research, and that without patient participation in current studies, there can be no new knowledge to benefit future patients.” Patient involvement in clinical research: Why, When, and How (José A Sacristán et al., 2016)
Other stakeholders exchange ideas, share experiences, and connect new information into a meaningful framework for others. (See articles re: whistle-stop tour, physician panel proposal, Kidney Week 2018). Yet current corporate and industry practice seems isolated and mired in taking past experiences to overlay assumptions on new efforts, rather seeking new approaches and using a collaborative approach to better inform their outreach and efforts in the aHUS arena.
Physician Interface: Who’s Networking?
The aHUS space has expanded and most stakeholders understand that it’s not just about nephrology, but an entire range of sub-specialities and multidisciplinary aspects. There’s wide variance among clinical sub-types of patients with atypical HUS, which compounds the many difficulties with diagnosis and treatment. Atypical HUS activity may affect organs other than the kidney and occur as acute episodes (distinct events, or lasting a short duration) or as an ongoing, chronic illness. People with the same genetic mutation can have distinct differences in presentation and aHUS medical histories, as well as differing symptoms and severity. With such a rare and complex disease, is it any wonder that physicians treating aHUS patients face multiple challenges? Where do physicians obtain accurate and updated information about atypical HUS? Is information about clinical trials and aHUS research easily available, or scattered across multiple platforms and buried on website subpages?
Clinical trials related to aHUS have faced serious recruitment and enrollment issues, even as companies involved keep depending on more traditional, well-traveled information pathways. Physicians gather in various groupings: within hospital divisions, in clinical teams or practices, at national medical events, and at regional or professional meetings. Scientific and ethical reasons exist for most clinical trials to focus on enrollment of people 18 years and older, as opposed to young patients, which explains why traditional communication flow may forget to include people or groups whose affiliations, credentials, or events include the tag ‘pediatric’. Pediatric physicians engage in collegial discussions and attend meetings to gain new information, which is then shared with other clinicians in a variety of settings. Summarily discounting the value of pediatric clinicians, hospitals, and symposiums disrupts connectivity within the information flow and clinical trial loop. Such limited thinking is a disservice to all, and acts as barrier in the clinical trial arena.
Communication is seldom a linear endeavor, and in the aHUS space it is more accurately viewed as networking relationships among diverse people and groups. Hospitals are often arranged by divisions such as hematology, nephrology, immunology, and other specialties, with information flow far beyond departmental meetings. New emphasis for multidisciplinary or thrombotic microangiopathy (TMA) care teams may impact management of aHUS, but this also provides opportunity for ‘MedEd’ events such as the August 2017 symposium on atypical HUS as a TMA (TMA Boston) which was co-chaired by pediatric nephrologist Dr Andrew Siedlecki and the aHUS Alliance team. Each of eight physician presentations were framed by aHUS patient experiences, such the eloquent statements of Michael Eygenraam of aHUS Canada prior to an outstanding clinical presentation by Dr Jean Francis of the BU School of Medicine (Watch: Time Stamp 2:36 of this video).
Many dedicated physicians have offered insight into the difficulties they face regarding aHUS diagnosis, treatment options, and case management. The complement inhibitor eculizumab, currently the only drug approved for aHUS treatment, is available to less than a quarter of nations (‘over 40 nations’ according to Alexion Pharmaceuticals, corporate list). Since approximately 75% of nations do not have access to this drug, simple market economics mean that these ‘underserved’ countries may form prime targets for those with new aHUS therapeutic drugs in development. Such concerns are apparent in journal articles such as Orphan drug policies and use in pediatric nephrology (Karpman D and Höglund P, 2017). A closer look at IPNA Bucharest, organized by Dr Adrian Lungu with an ISN endorsed robust agenda encompassing genomics, immunology, and complement topics, shows a speaker roster from nations including Australia, Belgium, China, Germany, and Italy. Networking with specialists in nations with strong interest in aHUS, and particularly in countries without eculizumab, provides a starting point for to build relationships in diverse but related fields. (See our network: aHUS Clinicians & Investigators) Clinicians are on the front lines of what really happens in hospitals and exam rooms, leading to the proposal to address the current issues with aHUS drug access through a global review physician panel model for aHUS drug access. One measure of potential or predictive commercial success of an effective drug would be drug access and its corollary topic of drug cost, which is neither unique nor specific to atypical HUS. How much outreach is done with the professionals who lead conferences, give clinical presentations, or author research papers related to atypical HUS topics?
No matter how wonderful an orphan drug might be in regard to its ability to save or transform patient lives, what value does it retain in parts of the world where market conditions or high cost make the drug unavailable to physicians and their patients? It’s unlikely that current barriers to aHUS clinical trial enrollment will be overcome without new approaches to physician outreach and communication.
Connecting Fragments to form Solutions
There are multiple barriers to launching and enrolling clinical trials, particularly with rare diseases such as atypical HUS. Fragmented information flow is a key and pervasive issue, along with other aHUS market factors outlined in detail within our 2018 aHUS Alliance pharma overview. Needs or areas of concern clearly stated by patient organizations and physicians somehow have not risen to the attention of industry. Why the disconnect, and on so many topics?
Background information on aHUS clinical trial needs and concerns is available through multiple outlets, and the aHUS Alliance frequently compiles information and updates in our ‘trials watch’ and ‘pharma overview’ articles as well as in frequent social media posts on Twitter and Facebook. As an independent and objective voice of aHUS advocates around the world, aHUS Alliance volunteers have continued to indicate our interests and concerns. The aHUS Alliance has identified as stakeholders having keen interest in atypical HUS studies and clinical trials such as: national aHUS patient organizations (click HERE), aHUS clinicians and investigators (click HERE), and various aHUS and TMA study centers (for a partial list, click HERE). What’s indicated when physicians and advocates clearly state insights and avenues, yet hear from professionals in communications and industry that they’re running up against barriers that we’ve already identified? Shouldn’t professionals experienced in markets and clinical trial aspects be aware of assets in the aHUS space, to use as a launching pad to better inform their effort?
The aHUS Alliance anticipates that barriers in the aHUS clinical trial space will continue to be problematic until and unless issues we’ve raised are addressed. When will detailed information about clinical trials, and the status of their current progress, become easily found and no longer necessitate clicking through subpages as one visits multiple research sites, medical journals, and corporate websites? How can aHUS patients and advocates play a more robust role in research? When will the physician voice be not only heard, but their experiences understood and solicited in a meaningful interface that fosters both advancements in knowledge as well as resulting in broadly available and effective aHUS treatment options? The aHUS Alliance remains dedicated to the concept that good will come together, through dialogue and collaborative efforts among stakeholders to build a brighter future for aHUS patients and their families around the world.
L Burke

Notes:
Visit the Resource section of our Info Center for an updated directory of more key original content on these topics.
The aHUS Alliance welcomes contacts from clinicians, academic or research teams, and those developing or leading clinical trials relevant to atypical HUS.
Reach out to the aHUS Alliance at info@aHUSallianceAction.org

18 Oct 2018

