4 MYTHS of Rare Disease Advocacy: Digging deeper into Common Misperceptions
Pathways of Patient Engagement & Recruitment
The THIRD Article in our Four Part Series
Although there are over 7000 rare diseases, rare patient populations affected by each are by definition very small numbers of people. In nations around the world, people living with a rare disease become advocates to help raise awareness, share information, offer insight, provide support, assist research, and promote healthcare policies that make a positive difference. Depending on the situation, people, and groups involved there’s both an art and a science behind effective advocacy and patient engagement in the rare disease arena. At the same time, proactive avoidance of common pitfalls to may help ideas and projects to bypass ‘echo chambers’ that fail to optimize efforts and maximize results.
The term “rare disease” might mislead the general public as an estimated 350 million people are living with one of these rare diseases, with perhaps many more people still undiagnosed or misdiagnosed. Rare disease statistics, definitions, and other information varies around the world. In Europe, a disease or disorder is defined as rare when it affects fewer than 1 in 2000 people while the USA definition is slightly different, defining a disease or disorder as rare when it affect fewer than 200,000 Americans at any given time. (Source – Rare Disease Day: What is a Rare Disease )
Patient populations of any rare disease groups are small, so patient engagement and recruitment needs to follow particular & specific pathways to conduct surveys or to involve patients.
It would be highly unusual if rare disease patients were simply interested in the medical aspects of their diagnosis. Patient lives are challenged by social and emotional impact on themselves and those surrounding them, often with a substantial economic burden and change in lifestyle for the whole family. Multi-discipline approaches to care teams are gaining favor (Gordon C et al, 2017), as physicians move toward rare disease models that are more holistic. Depending on their location and available heathcare resources, aHUS patients might be referred to a hematologist, nephrologist, or immunologist. Twenty percent of patients with atypical HUS have no kidney issues (De Yao J et al, 2015), but thrombotic microangiopathy (tiny clots in small blood vessels) affecting organs throughout the body means that aHUS patients may experience extra-renal Involvement and require specialist intervention for issues related to the heart, lungs, GI sytem, skin, or eyes (Hofer J et al, 2014) . Nutrition and mental health are slowly being recognized as integral components of patient health. Not all patients with a particular rare disease present at medical appointments with identical symptoms and circumstances, and it’s not unusual for multiple complexities to shade treatment plans.
In patient recruitment there remains an unmet need to account for clinical heterogeneity, or variations among patient experiences. Subsets of patients exist in every rare disease group, but it’s not often that this is recognized when people craft outreach efforts. In the case of people living with atypical hemolytic uremic syndrome (aHUS or atypical HUS), clinical subsets are numerous and with great variability in terms of characteristics and needs. Including subsets from rare disease groups will produce wider insights and more accurate data. The atypical HUS patient population is almost evenly split in number between adult patients and pediatric patients, with clinical subtypes for aHUS to include patients on long-term dialysis, transplant patients and pediatric patients. Geographic location and year of diagnosis also makes a difference, since some patients live in regions where the single drug currently approved for aHUS (eculizumab) is not available. Many patients were diagnosed with aHUS long before any therapeutic drug came to market, providing unique patient experiences and insights. Some people living with atypical HUS experience what seems an unending string of atypical HUS activity, while others have few episodes. Consider these two examples from the 2016 aHUS Alliance Global Poll. Are there more effective pathways to pursue for outreach and recruitment for rare disease surveys, clinical trial recruitment, and research efforts?
Survey Question 29 Participation in aHUS Research (Effectiveness of Patient Engagement. Would more patients participate in rare disease research if they knew how?)
36% – Would like to participate in research, but do not know how (aHUS Alliance, 2016 global poll, N=233)
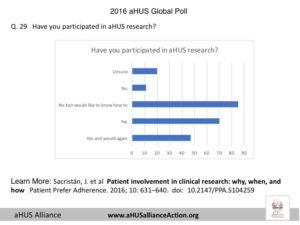
Sacristán J et al 2016. Patient Involvement in Clinical Research: Why, When, and How
Survey Question 34 Outreach & Recruitment for Patient Engagement: What might encourage greater patient participation in research studies or clinical trials? (Source: aHUS Alliance, 2016 global poll, multiple response question, N=233)
52% – Wider offering of opportunities to receive information and updates about ongoing studies or trials
48% – More information from my (our) medical team regarding current or ongoing studies or trials
47% – Inform patients how their participation can benefit their own care, help other patients and/or their own family members
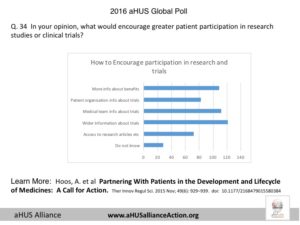
Hoos et al 2015. Partnering With Patients in the Development and Lifecycle of Medicines: A Call for Action
Given low patient numbers for any rare disease it’s difficult to find and engage a wide variety of patients, but critical disease characteristics such as genetic variants of atypical HUS may have potential to influence treatment effectiveness. BK Potter and team in 2016 noted, ““Research to evaluate the implementation of new therapies in real-world settings must respond to an evolving set of existing interventions and care pathways as well as consider the roles of multiple decision makers, including clinical providers and policy makers along with patients and families.” That’s one aspect, but currently much value is being left on the table, with patient organizations sometimes being contacted out of thin air by individuals asking for very specific assistance but with little information offered about the initiative, those leading it, or how the effort may benefit patients or add to advancements in research. In their 2014 review of approaches for engaging patients for research on rare diseases, Dr. Laura Forsysthe and team noted no one reported training researchers in engagement methods and, “in four studies, patient organizations were engaged only for providing access to their members.”
Somehow marketing specialists and survey tools have not embraced realistic views of what living with a rare disease really means to patients and their families. Undertaking market research faces constraints and knowledge of the both existing landscape and understanding of future directions for advancements. New methodologies are needed to design effective outreach and to optimize initiatives that engage the rare disease community and its small patient populations. Sound reasons exist as to why clinical trial stages include pediatric patients after proof of concept demonstrates feasibility and drug safety, and with interim data available to effectiveness for adult patients with a rare disease. Yet some of the most active physicians involved with medical conferences and posting actively on social media are those who treat pediatric patients. Think creatively. Why aren’t those conducting surveys, marketing, and research programs recognizing that networking is not linear? While studies or therapeutics suitable for pediatric patients may be further in the future, it’s never to early to start the connectivity that should be at the heart of engagement. Most doctors are part of a larger network of clinical or hospital staff who meet regularly or informally to discuss cases and treatment advances, and many are part of medical interest or professional groups that include doctors who connect with other specialists. What effect might it have if rare disease patient organizations were invited to preview survey tools prior to launch? How might survey methodology change if those leading that effort realized rare disease patients who experience kidney function issues often deal with fatigue but also may experience ‘brain fog‘ or cognitive functioning issues which may affect clarity or memory?
Adult patients may be too busy earning a living, or experience chronic illness that makes advocacy difficult. That does not mean that they’re not interested in participating in research or with surveys, it simply means that those conducting research programs need to think creatively and move beyond the traditional paths of patient engagement and recruitment. Can patient organizations play a role in this? Certainly, but know that most rare disease patient organizations rely heavily on volunteer efforts. Sadly it’s been far too common for people to contact these small groups of dedicated volunteers, and then discovery is made that ‘data mining for profit’ is at the heart of that contact. This is troubling on a number of levels, but it also creates a barrier for those conducting valid research programs and survey efforts. These issues can work both ways. Industry, academics, and researchers can look at the public content of rare disease advocacy outlets to help determine viable paths for engagement. Is the content of certain websites or social media nation-specific, or does it indicate an awareness of patient issues and disease-specific efforts globally? Is the material posted by an individual advocate or patient organization indicative of broad-based interests and connections with physicians and researchers? Are the informational resources the rare disease patient organization well developed and useful to wide audiences, complete with citations for fact-based content or credit for sources? Perhaps this may be surprising to some, but for many patient advocates and patient organizations money isn’t the prime motivator for patients to participate in marketing surveys. Rare disease patients and advocacy groups recognize their unique ability to promote advances in research and medical treatment by helping to provide patient-centric data through participation of individuals affected by the rare disease. As evidenced by data from the 2016 aHUS Global Poll, patients want to be included in research efforts, but may not know how and are not confident that their physicians are well updated Be wary of any group or organization that doesn’t include statements of how participation in study or survey may advance treatment or research for their rare disease, or if there’s a general call for “someone, anyone” on recruitment or market research efforts. Poor survey methodology, flawed study design, or ineffective outreach does not make for reliable data on which to develop therapies or to base decisions about programs. There are valid reasons behind that old saying among analysts, “Junk in, junk out“.
In her 2016 BMJ editorial Co-Production: A New Lens on Patient-Centered Care, Madge Kaplan refers to the idea of co-production, and how patient involvement figures in this concept. Kaplan notes the term co-production arose from 1960s era economists who observed that the USA service economy in sectors such as retail and education were structured differently and needed a new approach as opposed to past practices within industrial economy sectors of manufacturing and agriculture. In her article, Kaplan wrote about research done by M Batalden et al in Coproduction of healthcare service , “Batalden acknowledges that co-production is similar to patient engagement initiatives and partnerships growing around the world. The difference is that patient and family advisory panels, for instance, sometimes function like a manufacturer holding focus groups to get customer feedback on a new product. Co-production means having patients on the design team co-creating improvement programs from day one.” Below is a diagram from that research article of Marie Batalden and team (2016), which indicates this broad concept of collaboration and notes, “Efforts to ensure effective participation of patients in healthcare are called by many names—patient centredness, patient engagement, patient experience. Improvement initiatives in this domain often resemble the efforts of manufacturers to engage consumers in designing and marketing products. Services, however, are fundamentally different than products; unlike goods, services are always ‘coproduced’. Failure to recognise this unique character of a service and its implications may limit our success in partnering with patients to improve health care.”
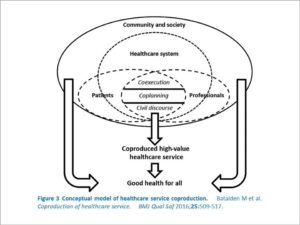
By whatever terminology or yardstick of success for patient engagement concepts and projects, it’s clear that a focus on collaboration and new pathways need to be considered prior to the launch of initiatives. Approaches within the rare disease arena may stagnate within unproductive echo chambers, so small patient numbers need to be proactively considered as an opportunity to network and maximize potential to gain authentic and meaningful input. Given the small numbers of patients of any given rare disease present special challenges, especially when there is much clinical heterogeneity, pathways for communication and recruitment must be thoughtfully constructed to allow for broad, effective engagement of both patients and physicians.
L Burke, Jan 2018
For More on the topic of aHUS Market Factors, Patient Recruitment, and Clinical Trials see
2020 aHUS Alliance Report:
2020 Atypical HUS Therapeutic Drug Landscape – an Overview
https://bit.ly/aHUS2020drugReview
2018 Therapeutic Drug Pipeline & Market Factors May 2018

This is the third in an aHUS Alliance 4 part series released over four weeks, with its entirety referencing material noted below. Take a closer look at these topics:
Organized groups such as national patient organizations are the only place where individual advocates can make a difference. (Click HERE to read Part 1 of 4 topics)
The best way for rare disease patients to be an advocate is to share their personal journey and patient experiences. (Click HERE to read Part 2 of 4 topics)
Patient populations of any rare disease groups are small, so patient engagement and recruitment needs to follow particular & specific pathways to conduct surveys or to involve patients. (The Article you are Currently Reading)
Patients Included: Rare disease patient advocates are invited participants at almost all healthcare and medical conferences. (Click HERE to read Part 4 of 4 topics)
Resources & Citations
Dharssi S, Wong-Reiger D, Matthew H, and Terry S. Review of 11 national policies for rare diseases in the context of key patient needs
Orphanet J Rare Dis, Mar. 2017.
Morel T et al. Quantifying benefit-risk preferences for new medicines in rare disease patients and caregivers. Orphanet J Rare Dis, May 2016.
Robinson R. Patients and Patient Organizations Power Rare Disease Therapies. PharmaVoice.com FE 2016
Merkel et al. The partnership of patient advocacy groups and clinical investigators in the rare diseases clinical research network. Orphanet Journal of Rare Diseases May 2016
The Origins of Patients Included Patients Included: Charter
Forsythe, L et al. A Systematic Review of Approaches for Engaging Patients for Research on Rare Diseases J Gen Intern Med. Aug 2014
Potter BK, et al. Translating rare-disease therapies into improved care for patients and families: what are the right outcomes, designs, and engagement approaches in health-systems research? Genet Med. 2016
Editioral, Vivisum Partners: corporate marketing blog Junk In, Junk Out: The Consequences of Poorly Designed Survey Instruments Apr 2014.
Utengen A et al. Patient Participation at Health Care Conferences: Engaged Patients Increase Information Flow, Expand Propagation, and Deepen Engagement in the Conversation of Tweets Compared to Physicians or Researchers. J Med Internet Res, Aug 2017


