Anyone, who has been involved in aHUS patient advocacy for some time, will be aware of the special place that those patients, whose aHUS has left them with chronic kidney failure, and are dialysis dependent ,have in the aHUS community .
Prior to the advent of eculizumab, this was the state that many of those now accessing eculizumab would have been in, if they had survived their encounter with aHUS.
For those that did end up on dialysis ,however , it was the double blow that having a kidney transplant to help them recover was a trigger of aHUS ; and it would mean almost always the destruction of their kidney graft. It was also almost a universal clinical protocol that, without a complement inhibitor, dialysis patients would have to remain on dialysis for life and would not be eligible for a transplant.
Eculizumab provided the opportunity for that to change, and dialysis patients could look forward to a kidney transplant and get on the transplant list.

Kelly of Castle Dale Utah USA asks “Will my status on the transplant list be lower because I have to be on eculizumab. Will they pass me up for a patient that does not have aHUS?”
Criteria for being accepted to a list for non living kidney donor transplant lists vary by country, but the aHUS alliance is not aware of any which exclude , or reduce priority for , aHUS patients where the transplant is to be supported by funded eculizumab. Tissue type match and waiting days on the list usually determine the order of selection , Kelly.
The work of the Zuber Group in France, based on a French aHUS transplant cohort, set the standard for aHUS transplant protocols . Those who were to receive a living donor kidney could be prepared ahead of the transplant operation and hit the ground running, so to speak, as far as complement blockade was concerned.
But, as the Rare Disease Day video questions show, in some countries dialysis patients were to face further discrimination as health policies were put in place that dialysis patients remained outside the scope of eculizumab unless they experienced another aHUS episode, even one triggered by a transplant.
Except for women who are predisposed to aHUS choosing to become pregnant , aHUS dialysis patients face a scary decision about transplant, particularly as they have already experienced what aHUS can do. They are also having to decide, without adequate evidence of the likelihood of aHUS recurrence; and what damage would be done if it did re-occur.
.
Ashley of Victoria Australia asks “Are there any studies being done about the effectiveness of eculizumab in transplant patients and will there be data available to persuade the Australian Government to fund eculizumab for transplant patients”
Ashley, this is why the aHUS alliance proposed research into transplant outcomes as a top priority for the Global aHUS Registry; and it became the No 1 priority project in the Registry’s Scientific Advisory Board research programme.
A small group of top aHUS researchers from Australia, Belgium and the USA has been set up and have begun to look at transplant outcomes of those enrolled in the aHUS Registry the largest number of aHUS transplant patients for which data is available.
The alliance has been given an update from one the investigators Dr Andew Seidleki of the Harvard Medical School ( the alliance had previously featured the groups preliminary report at the ASN’s Kidney Week see here)
- those transplant patients with a diagnosis of aHUS receiving eculizumab before or on transplant day 1 had much less need for dialysis post transplant than those who did not.
- those transplant patients without an aHUS diagnosis prior to transplant ,but who onset post transplant, responded well when eculizumab was introduced.

Kelly of Ipswich Queensland Australia asks ” Thanks to the new drug eculizumab and after 18 years on dialysis I am currently being assessed for a kidney transplant . Would n’t it be better to take eculizumab straight after transplant instead of waiting for aHUS to recur . I am quite scared at the thought of the aHUS coming back?”
So Kelly the preliminary results of the aHUS Registry have found it would be better to receive eculizumab than not to receive it on transplant ; but those did not receive it because they had not been diagnosed with aHUS until the transplant triggered aHUS look like they recovered well when aHUS re-onset and eculizumab was introduced.
Having had a successful transplant supported by eculizumab before or after the operation the question becomes one of whether eculizumab can be withdrawn particularly with the kidney graft being a potential trigger of aHUS for life.
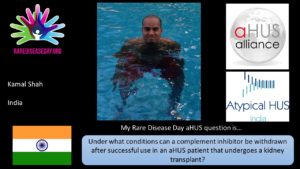
Kamal of India asks ” Under what conditions can a complement inhibitor be withdrawn after successful use in an aHUS patient that had undergone a kidney transplant”
It should be a clinical decision based on the risks likely for an individual patient. When such a decision is made should be on clinical evidence and not be determined by an arbitrary date as Anne -Sophie of Belgium asks “I have had aHUS Factor H for 13 years and have been on dialysis since then . When I will be transplanted only in Belgium do you receive eculizumab for 6 months. Why do I have to be sick again to receive it again.”

First do no harm is a principle underpinning health care, so at a minimum there should be a care pathway for those in Belgium facing this arbitrary decision with a means to self monitor and identify any returning TMA activity at the earliest opportunity.
But the answer to those questions should be part of what is found out about withdrawal from eculizumab studies going on around the world see previous blog click here

