
As sometimes happens in life, things can arise as a group that makes people take a bit more notice than if they’d had singular appearances. In medical circles, it’s not all that common to read publications that make readers feel there’s potential to make a lasting impact on the way physicians treat people with rare medical conditions. Yet that’s where we seem to have landed, as we offer this June 2024 overview of recently published articles specific to atypical HUS.
There are still many knowledge gaps across aHUS topics, and it’s important for patients and their families to understand that there are areas which continue to be debated by the experts. People who are genetically predisposed to aHUS may experience their first episode of disease early or quite late in life, with potential multi-organ damage from symptoms that can vary greatly in severity and duration. Much is unknown about how certain circumstances regarding genetics and environmental factors may combine to trigger atypical HUS disease activity, such as: infections (bacterial/viral), pregnancy, certain drugs, organ transplantation, cancer, and inflammation or chronic/autoimmune disease impact. As research progresses, perhaps we’ll also gain more understanding to fill knowledge gaps that in turn may shed light on ‘idiopathic’ cases – people diagnosed with atypical HUS who do not appear to have any underlying cause or genetic factors.
Experts: Not always in Agreement
That aspect leads us right to a very important new publication, The role of complement in kidney disease: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference (Vivarelli et al, 2024). In 2022 a panel of experts met in Italy to discuss ‘The Role of Complement in Kidney Disease’ and this publication is its result. This 70 page document covers the spectrum of issues related to the diagnosis and treatment of kidney diseases such as aHUS, C3 glomerulopathy, and more. (FMI on its impact, read our overview.) Know that these KDIGO guidelines will guide doctors and clinical practice around the world. Know also that there’s a reason for the term ‘controversies’ in the title. Simply put, there are many ‘gray areas’ and knowledge gaps with differing opinions among experts.
Controversy cropped up again in an exchange noting that experts in atypical HUS, also known as ‘complement mediated Thrombotic Microangiopathy’ or cmTMA, are not always in agreement. The titles alone illustrate this point:
Maritati et al. “Eculizumab First” in the Management of Posttransplant Thrombotic Microangiopathy
Maritati et al. Response to “A Caution Against the Use of C5B-9 Endothelial Assay to Support Eculizumab Therapy”
Points to Ponder
People may be taking a second look at previous knowledge when considering the aspects that touch upon the topic of diagnosis and of onset age’s potential effect on patient outcomes. The publication by Cole et al utilized a modified Ham test (mHam), an assay to detect abnormal complement activity in a variety of complement diseases, and took it a step further. Wouldn’t it be great to have better tools to help diagnose atypical HUS? That seems to be indicated with the work of Cole et al. Complement Biosensors Identify a Classical Pathway Stimulus in Complement-Mediated Hemolytic Uremic Syndrome regarding complement ‘bisensors’.
If there was a way to quantify the body’s ramping up and dysregulation of the complement system, could that not only improve aHUS diagnosis, but also impact clinical abilities to monitor patients using complement inhibitor drugs? That would be a most welcome advancement as a game changer, and it’s been announced that “…we have developed an array of cell-based complement “biosensors’’ by selective removal of complement regulatory proteins (CD55 and CD59, CD46, or a combination thereof) in an autonomously bioluminescent HEK293 cell line. These biosensors can be used as a sensitive method for diagnosing CM-HUS and monitoring therapeutic complement blockade.”
Also of interest was data provided within the publication by Celegen et al. Adolescence-onset atypical hemolytic uremic syndrome: is it different from infant-onset? This study included 28 patients, and seemed to indicate that adolescent-onset patients experienced more permanent issues with kidney function than those whose aHUS first occurred as infants. Interestingly there were 21 girls and 7 boys in the study cohort, all between the ages of 10 and 18 years old. We wonder if gender or puberty may play some role as well, but as researchers often note, “That would need further study”.
aHUS & Pregnancy – Doubling Down
In a relatively short time frame, there’s been an unusually large grouping of publications released lately which have been related to health issues in pregnant women with atypical HUS (aka cmTMA) and other forms of thrombotic microangiopathy (TMA) Although the varying terminology may make it difficult to follow, women diagnosed with cmTMA and other TMAs may experience complex health concerns during any stage of pregnancy, to include postpartum care.
We’ve long been advocates for multidisciplinary care teams and that’s never more true than in conjunction with pregnancy, given that tiny clot formation can occur anywhere in the mother’s body (to include the placenta) and may in some cases cause concern for fetal health as well. Despite a mother’s complex care challenges that accompany any TMA diagnosis, healthy pregnancies certainly can and do occur, with many healthy babies launching joyous beginnings within their new families.
Sixteen new publications specific to aHUS/TMA issues just have been added to existing 2024 and prior articles within our virtual library’s category for pregnancy. We’ll highlight one in particular, Urra et al. Thrombotic Microangiopathy in Pregnancy: Current Understanding and Management Strategies. Two of the co-authors names may be familiar to families who have heard presentations by Dr Anuja Java at an aHUS meeting, or have read our interview with Dr Richard Burwick who is a specialist in Maternal-Fetal medicine.
This article provides an overview of pregnancy-associated thrombotic microangiopathy (p-TMA) regarding information pools that intersect the varied group of disorders that can challenge appropriate diagnosis and treatment.Identifying the various forms of thrombotic microangiopathies needs to be done rapidly but accurately, in sorting out preeclampsia from HELLP or whether the diagnosis might be from other clinical entities such as aHUS, APS, or TTP. (Figure 2)
This publication also addresses the ‘when’ aspect of onset and its potential differences in treatment or outcomes, since women may have an existing aHUS diagnosis prior to pregnancy, trigger during the different trimester stages, or have TMA occur at/after delivery (postpartum). Indeed, such variations in patient profiles are the focus of several other recent publications noted below.
Altaf et al. Successful Management of Atypical Hemolytic-Uremic Syndrome in Pregnancy Using Eculizumab: A Case Review DOI: 10.7759/cureus.57973
Barrera-Hoffmann et al. Pregnancy-associated atypical hemolytic uremic syndrome. Case report DOI: 10.1111/jog.15958
Che et al. A case-based narrative review of pregnancy-associated atypical hemolytic uremic syndrome/complement-mediated thrombotic microangiopathy DOI:https://doi.org/10.1016/j.kint.2023.12.021
Domínguez-Vargas et al. Pregnancy-Associated Atypical Hemolytic Uremic Syndrome: A Case Report with MCP Gene Mutation and Successful Eculizumab Treatment doi: 10.1055/a-2164-8438
Kaufeld et al. Features of Postpartum Hemorrhage-Associated Thrombotic Microangiopathy and Role of Short-Term Complement Inhibition DOI: 10.1016/j.ekir.2024.01.035
Krelle et al. The Challenges of Distinguishing Different Causes of TMA in a Pregnant Kidney Transplant Recipient DOI: 10.1155/2024/9218637
Komatsu et al. Severe hemolysis, elevated liver enzymes, and low platelet syndrome requiring differentiation of thrombotic microangiopathy: Four cases from a nationwide survey in Japan https://doi.org/10.1111/jog.15949
Korotchaeva et al. Eculizumab for pregnancy-related atypical hemolytic uremic syndrome DOI: https://doi.org/10.1093/ndt/gfae068
Miyazaki et al. Pregnancy-Associated Atypical Hemolytic Uremic Syndrome Successfully Treated with Ravulizumab: A Case Report DOI: 10.7759/cureus.54207
Okawa et al. Plasma Exchange in Postpartum Hemorrhage (PPH)-Associated Thrombotic Microangiopathy (TMA): A Case Report DOI: 10.7759/cureus.59623
Perez et al. Atypical uremic hemolytic syndrome diagnosis, therapeutic management, control and follow-up in pregnancy: about a case DOI: https://doi.org/10.1093/ndt/gfae069.1288
Urra et al. Thrombotic Microangiopathy in Pregnancy: Current Understanding and Management Strategies DOI:https://doi.org/10.1016/j.ekir.2024.05.016
Van Gendt et al. Pharmacokinetics of Monoclonal Antibodies Throughout Pregnancy: A Systematic Literature Review DOI:https://doi.org/10.1016/j.ekir.2024.05.016
Yasmin et al. Protective role of complement factor H against the development of preeclampsia DOI: 10.3389/fimmu.2024.1351898
Venou et al. Increased Complement Activation and Decreased ADAMTS13 Activity Are Associated with Genetic Susceptibility in Patients with Preeclampsia/HELLP Syndrome Compared to Healthy Pregnancies: An Observational Case-Controlled Study DOI: 10.3390/jpm14040387
There’s a whole world of information to explore, click below to view hundreds of publications organize by topic
Atypical HUS Research & Publications
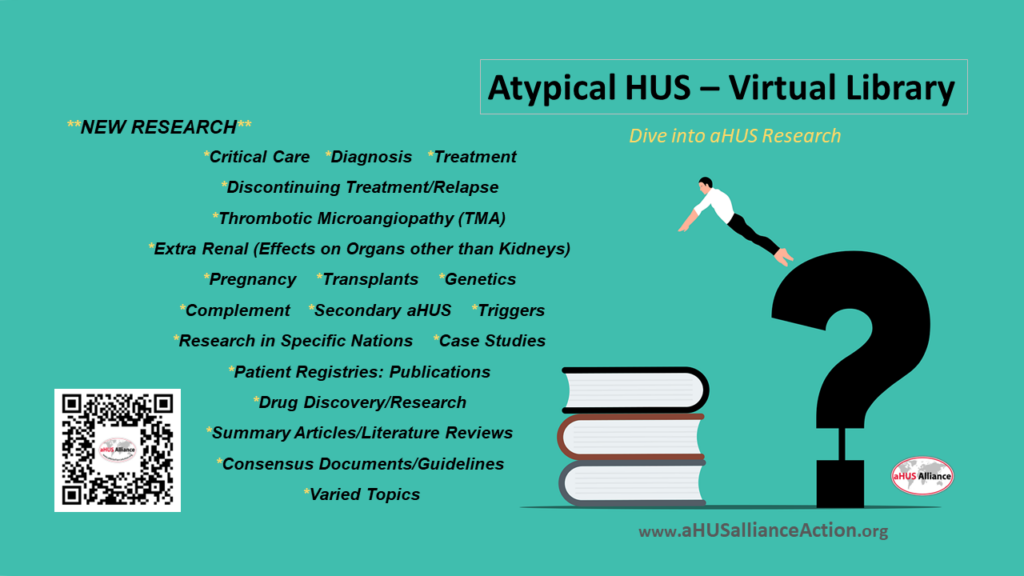
Research articles about atypical HUS are listed within our website on topic-specific lists within our Info Centre, with the most recent added to the “New Research” scroll as well as listed in date order within each topic category.. Click the jump links at the top of the Research & Publications page to skip down to a category of interest.
Visit our Research & Publications page, a ‘Virtual Library’, a resource created and maintained by
the aHUS Alliance Global Action team
Note: Spot a great publication that should be added, or wish to provide feedback about this virtual library? Please contact the curator at E: Linda@aHUSallianceAction.org

