These days a kidney transplant may not feature much in the thoughts of new onset aHUS patients, most of them can be saved from a life of chronic end stage kidney failure by eculizumab. Some however are still falling through the safety net and joining those aHUS patients who have been living a life on long term dialysis for some years.
So the topic of kidney transplant treatment strategy for aHUS patients still features in the aHUS Patients’ Research Agenda with the specific question:
Is there a significant difference in outcome between having a complement inhibitor before or after a kidney transplant?
Indeed the aHUS alliance affiliates regarded answering that question as the top priority for research.
They did so because firstly there are a substantial number of aHUS patients still on dialysis, even though eculizumab is available to them to have a transplant.
Secondly aHUS dialysis patients are often left outside of the scope of eculizumab access unless their transplant triggers a new TMA. They are also facing limited access for an arbitrary period, sometimes as little as six months, even though their transplant remains a trigger for TMA. A policy which has been faced by patients in countries like Belgium and Australia.
In late 2015 the alliance told the Scientific Advisory Board of the Global aHUS registry that aHUS patients needed to know whether it was better to have a transplant with eculizumab and if it was better whether there were advantages to health if it was given before or after the operation? Implicit within that is whether it is better for the patients if its given before another TMA is triggered.
The SAB made it the top priority in its research programme. A research project team was given the task to find answers.
It has taken some time do it and the alliance has reported about it on several occasions over the past year as information about the task group’s findings was released in posters and talks at important renal conferences..
At its meeting in Nijmegen the alliance was given a preview of the research finding by one of the authors, Prof. Johan van de Walle ,thus completing the circle on this task as far as the alliance is concerned.
On 18th December the research was published in “Kidney International” , the International Society of Nephrology’ (ISN), prestigious journal. It is free to view and can be read by aHUS patients by clicking here
It is truly an international effort, the key authors ,including lead author, Andrew Sedilecki from Boston, who collaborated with the alliance in the TMA Boston symposium ,are from the USA, Australia and Belgium.
It is also the largest number of aHUS transplant patients studied, which could not have been done without them participating in the Global aHUS Registry.
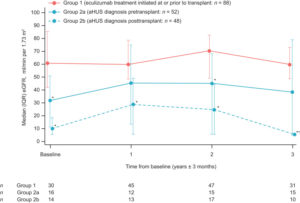
The alliance does not intended to precis the publication, the article ( at the link given above )is fairly clear and understandable. However one graph says a lot about the concluding message.
The alliance’s observations on what this “says” follow:-
The red line shows the kidney graft performance ( Estimated Glomerular Filtration Rate (EGFR) for those diagnosed aHUS patients accessing eculizumab prior to their kidney transplant operation. On average the graft kidney function is at 60% of normal function and this is with one kidney . Some transplanted aHUS patients were achieving performance levels of 80%. By normal transplant standards this is a very good outcome for someone.
The continuous blue line shows the kidney graft performance for diagnosed aHUS patients receiving eculizumab once the transplant triggers a new TMA. On average, performance of those new TMA damaged graft kidneys starts off much worse at 30% on average , with some much lower in the early days sometimes with inadequate kidney function needing supplementary dialysis. However the performance begins to improve, reaching 40% of normal function with again just one kidney. Some patients can get even better performance but some do not really recover much from the damage done by the new TMA. It is however on average a better outcome from being on chronic kidney dialysis, but poorer than those getting prophylactic ,rather than rescue, eculizumab therapy.
The dotted blue line shows the kidney function of those patients who were given a kidney transplant but whose original kidney failure had not been identified as caused by aHUS. Their diagnosis becoming known sometime after the transplant triggers a TMA. Their graft kidney performance is just above the level of end stage renal failure and they need acute kidney dialysis treatment. Once, sometime later ,they get a proper diagnosis and eculizumab rescue therapy begins, the damaged graft improves its performance but only to 20% of normal function on average, though some can do better Some patients’ function remains so low that a return to dialysis is needed . For those hopefully not too much damage is done by the transplant that another kidney transplant can be performed with the knowledge that a TMA is very likely without eculizumab.
Putting it very simply those diagnosed with aHUS and getting eculizumab before a transplant on average have twice as good a clinical outcome than those diagnosed but only allowed it on recurrence of aHUS.
But those diagnosed with aHUS, getting it as a rescue therapy once a TMA is triggered, get twice as good a clinical outcome as those undiagnosed and then newly on-setting with aHUS following transplant . Also these diagnosed patients fare much better than if they stayed on dialysis.
Finally those not properly diagnosed before the transplant but finding out after, on average fare little better than those on dialysis, though some can do much better, and are likely to return to dialysis and need another transplant if that is now possible. On average their outcome is little better than those aHUS patients who had kidney transplants in the past before eculizumab was ever thought about as a treatment.
So those aHUS patients facing a transplant can use this to have a dialogue with their clinicians to see what eculizumab prescription strategy they are thinking of, prophylactic or rescue, and talk about this evidence of relative outcomes.
Those patient organisations in countries which only permit rescue therapy following transplant now have some statistical evidence to have a proper challenge to such a policy.
Equally if only rescue therapy is available then patients need to know to weigh up whether an acceptable, but not great, kidney function outcome is better than staying on dialysis. Cognisant that it is also not impossible to get more than 50% function, which is as much as could be expected from one kidney.
Those undiagnosed at present but facing an aHUS onset on transplant can only be helped by research into aHUS diagnosis. That is another topic in the aHUS Patients’ Research Agenda. As too the wisdom of withdrawal of eculizumab from those with transplants is a question to be answered by another topic on our Agenda.
The alliance will be putting links to this article on its Facebook page so that those in the aHUS community can comment and ask questions.

