Article No. 308
5 January 2020
Issues surrounding the Switch from Pediatric to Adult Nephrology Care
It’s rewarding to watch children grow into fine people living happy, meaningful, and healthy lives. For those those with kidney disease and especially for families whose children have one of the over 7000 rare diseases, the concept of ‘healthy’ is described on a different, sliding scale that has additional concerns. As children with kidney disease grow to become adolescents, their medical care often changes from a pediatric to adult nephrology care setting – what are common issues that surround this transition?
How big is the problem of kidney disease?
Numbers of people affected by kidney disease indicate the scope of the issue. Out of the world population of an estimated 7.5 billion people, a World Kidney Day 2019 editorial, noted kidney disease is recognized as a global public health problem, affecting over 750 million people worldwide. In a June 2018 collaborative report (ERA-EDTa, ISN, ASN) on the prevalance of kidney disease, “We estimate that over 850 million people worldwide have some form of kidney disease, which is roughly double the number of people who live with diabetes (422 million) and 20 times more than the prevalence of cancer worldwide (42 million) or people living with AIDS/HIV (36.7 million).” According to World Bank data based on the United Nations Population Division, in 2018 just under 26 % of the world’s population was children aged 0 (newborn) to 14 years old, or almost 2 billion children worldwide.
Statistics vary by organization or nations but the depth of concern about kidney disease is clear. “Out of the 7.5 billion people in the world, between 8 to 10% of adults have some form of kidney damage. The number of children with kidney disease is about 18.5-58.3 per million children. About 70% of children with kidney disease will develop kidney failure by age 20 years.” (World Kidney Day, on Chronic Kidney Disease: CKD). From the USA’s Center for Disease Control, “In the United States, more than 9,800 children and adolescents have kidney failure or end-stage renal disease (ESRD), and they rely on life saving dialysis or a kidney transplant. The prevalence of ESRD in children and adolescents increases with age, with a greater proportion living with a transplant.” (CDC, CKD Surveillance Program)
Needs & Situations Vary
Treatment access and healthcare coverage for kidney disease patients of all ages varies widely around the world. Examples from national and international sources point to broad common concerns of treatment access as well as economic burdens of chronic kidney disease.. “Over 2 million people worldwide currently receive treatment with dialysis or a kidney transplant to stay alive, yet this number may only represent 10% of people who actually need treatment to live. Of the 2 million people who receive treatment for kidney failure, the majority are treated in only five countries – the United States, Japan, Germany, Brazil, and Italy. These five countries represent only 12% of the world population. Only 20% are treated in about 100 developing countries that make up over 50% of the world population.” Additionally, “Between 8 and 10% of the adult population have some form of kidney damage, and every year millions die prematurely of complications related to Chronic Kidney Diseases (CKD). In England, according to a recent report published by NHS Kidney Care, chronic kidney disease costs more than breast, lung, colon and skin cancer combined.” (Kidney.org)
In his 2012 paper on the epidemic of pediatric chronic kidney disease F Assadi stated, “Globally, the prevalence of chronic kidney disease (CKD) stage II or lower in children is reported to be approximately 18.5-58.3 per million children.” The International Pediatric Nephrology Association (IPNA) gathered information for a 2018 publication on renal replacement therapy (RRT, such as dialysis or kidney transplant) in children worldwide, which included responses from “94 countries (representing 86.2% of the world’s population), with 84 (81.2%) having the means to provide RRT to children, given that there are no other limitations such as financial, social, or religious restraints.” It further states that for children around the world needing dialysis, “differences in healthcare organization and delivery at a national level, ethnic differences in disease prevalence and sociocultural variation in the approach towards congenital and chronic disease in children may add to the observed variation in incidence rate and access to RRT.” The USA’s Center for Disease Control noted, “In the United States, more than 9,800 children and adolescents have kidney failure or end-stage renal disease (ESRD), and they rely on life saving dialysis or a kidney transplant. The prevalence of ESRD in children and adolescents increases with age, with a greater proportion living with a transplant.” (CDC, CKD Surveillance Program).
For those with a rare kidney disease, diagnosis can be delayed, treatment options limited, and medical profiles more complex. As the name suggests, atypical hemolytic uremic syndrome (aHUS or atypical HUS) impacts kidney function and can affect the function of other major organs as well. With few visible symptoms and highly varied clinical profiles, people diagnosed with aHUS need to be vigilant in regard possible decline or loss of kidney function. Some people experience atypical HUS activity as episodic (acute and short-lived periods of disease activity) while other people diagnosed with aHUS find it expressed as an ongoing, chronic illness. Children with atypical HUS often are seen by pediatric nephrologists, with parents as family caregivers, but what happens when young children become teenagers and young adults? Responsibility for self-care becomes even more important for those who have a past history or current kidney disease and are ‘aging into’ independent lifestyles even as they ‘age out’ of pediatric care settings.
Self-management of the health care transition (HCT) perhaps is best viewed as a continuum for adolescents & young adults with chronic kidney disease or ESRD (end-stage renal disease), with focus on preparation regarding physical, psychological, family, or ecological factors. What are some of the varied viewpoints and key issues for young patients, family caregivers, and physicians surrounding transitions for adolescents with kidney disease?
Becoming a Teenager, It’s not Easy for Anyone!
Linking cause and effect to real life situations is a fascinating, and very familiar, topic for families with children. ‘Magical thinking’ is a wonderfully apt term, and one which doesn’t necessarily end when people reach young adulthood. A 2015 article by Ronald Mah regarding magical thinking and teens noted, “teenagers can be incredibly inconsistent and frustrating in their follow-through on substantial life decisions- illogical behavior despite logical processing. Sometimes they act as if a fairy godmother or unknown benevolent mentor will pop out of the mists to grant rewards, opportunities, and riches despite their having spent negligible investment of energy or effort towards earning them.” Many adults still would like to wish away problems or to magically see a path forward when problems arise. Who wouldn’t desire a simple, elegant solution to routine dislikes, areas of difficulty, or issues that seem insurmountable or ever-present?
Adolescence is a highly-charged, emotional time for teens to want to fit in with their peers, blending into the crowd, yet still striving to develop/assert their own unique personality. In a 2014 Psychology Today article on Surviving Your Child’s Adolescence, by Dr Carl Pickhardt notes that “adolescent growth toward young adulthood proceeds along two major psychological paths: establishing independence and developing individuality.” For those with a chronic illness, this presents unique challenges for both the teen and their families. Clinical psychologist Dr Lori Rappaport wrote a helpful article for parents on Coping with Childhood Chronic Illness, describing the stress, emotions, and coping techniques common to families of children with chronic/life threatening diseases. “Being included and accepted by their peer group is an important focus at this age. They may feel left out due to missing school and activities due to treatment or physical limitations. Parents may become overprotective, restricting them from activities with other children. While this is a natural reaction, it can interfere with the child’s independence and sense of mastery.” While no one can wish away kidney disease, ignoring it or not following medical advice can put teens and young adults at great and irreversible risk. This is particularly true for those whose kidney disease has required a specialized diet, dialysis, or a kidney transplant.
For young people with kidney disease, physicians and parents need to recognize that early conversations can help ease the transition from pediatric care into adult care settings. It’s important that medical aspects be addressed within a context that recognizes the social and emotional needs teens and young adults who experience a chronic illness, like many kidney diseases. As noted in an article on compliance in the Journal of Adolescent Health, “Adolescence is a period of transition from dependence to independence, when adolescents begin to adopt a multitude of new social and emotional roles and learn to cope with altered bodily functions. Adolescents with a chronic illness are constantly struggling with independence. At the same time, their illnesses often keep them tied physically, emotionally, and financially to their families.”
Generally, transition readiness components include medical, social/emotional, and self-care aspects. The first steps of transition taken by most parents and medical teams are usually dependent less on age than on the child’s abilities, whether their diagnosis is newer or long-standing, and whether their current medical status is fairly stable. (A Sadlon, Patient Transition Office at Children’s Health) Here’s are two assets for parents and family caregivers to begin their exploration about the basics of what’s involved with transitions from pediatric to adult care.
‘Becoming an Adult: Taking Responsibility for Your Medical Care’ a 6 minute video (Nemours, with Dr Jennifer LeCompte)
Click below to View
Becoming an Adult: Taking Responsibility for Your Medical Care
Important areas usually included in discussions regarding transitioning teens to adult care are checking their ability to provide information regarding: name and specifics about their condition, ability to relay a brief medical history, medicine types and dosage information, insurance information and navigation, knowing contact info for doctors and specialists,how to watch for signs/symptoms that might indicate a change in medical status, filling prescriptions and what do during a medical emergency.
Some physicians and hospitals have a transition team, offering tools for families. Here’s a sample checklist from the ‘Got Transition’ online toolkits.
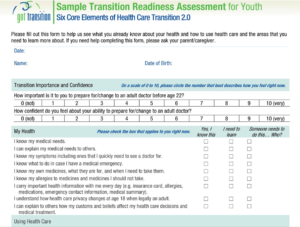
Click to View
Got Transition Toolkits: for Families, Youth, Physicians (also En Español)
Below are resources for families to explore aspects involved with transitioning from pediatric to adult care settings, and begin to consider how to awaken this teen self-awareness: the choice to ‘do their own thing’ starts with information about their kidney disease and knowing how to keep fit enough to do what they choose for personal goals and lifestyle.
RESOURCES
For Physicians
Khursigara et al. A Guide for Adult Nephrologists and Hematologists to Managing Atypical Hemolytic Uremic Syndrome and C3 Glomerulopathy in Teens Transitioning to Young Adults
Info & Resources for Families
Coping with Childhood Chronic Illness – article by Lori Rappaport, Ph.D. (Licensed Clinical Psychologist specializing in child and family issues)
Common Emotions, Adjustments & Coping Skills for children of various ages. A section on Siblings, as well as one on What Children want & need from Parents.
Chronic disease and the transition to adulthood: How to help your young adult feel empowered in their health care. (Patient Transitions, Children’s Health)
Adolescents with renal disease in an adult world: meeting the challenge of transition of care – Article – Varied situations & viewpoints of issues encountered when youth with kidney disease age into adult care units.
What is Healthcare Transition?: A ‘Got Transition’ Toolkit for Youth & Families (also En Español)
Info & Assets for: Discovering, Tracking, Preparing, Planning, Transferring, Completing.
Steps for Transitioning Pediatric Patients to Adult Healthcare How physicians can help families with transitioning teen patients. (Julianne Filion, Gebauer Co)
For Healthcare Providers: ‘Got Transition’ Toolkit: The Six Core Elements of Health Care Transition™ that define the basic components of health care transition support, to include establishing a policy, tracking progress, administering transition readiness assessments, planning for adult care, transferring, and integrating into an adult practice.
L Burke, 2020


