Here is a most unusual clinical article from earlier this year. In Thrombotic microangiopathies : An Illustrated review the Abou-Ismail Group explain TMAs using a series of illustrated images , almost comic strip like.
Starting with an explanation of what defines a TMA and the clinical features of a manifestation.
In the next page the “epidemiology”, annual incidence for 6 classified TMAs are given, with ranges showing how uncertain are the number of incidents each year.. Complement mediated HUS, as aHUS is called by some now, has the lowest incidence along with Hereditary TTP. The diagram is prefaced with the words ” TMA classification and nomenclature is challenging , as it lacks consensus and is constantly evolving” Something that Global Action has been saying for several years now and which reaffirms the direction of travel. ( https://www.ahusallianceaction.org/ahus-is-its-end-really-nigh-3/)
For one class of TMA, those triggered by drugs no attempt to estimate incidence is made but it is likely to be high.
This is followed by one of those charts which shows how to differentiate one TMA from another during the diagnosis process , including those four words of dread to the aHUS community ” clinical diagnosis of exclusion ” which sadly does not exclude enough and leads to some getting included incorrectly with other TMAs and misdiagnosed for too long.
( https://www.ahusallianceaction.org/an-ahus-diagnosis-lucky-or-what/ )
In the next two pages Thrombotic Thrombocytopenic Purpura, or TTP, is the focus. The immune mediated version ( where those autoantibodies are at it again) and the rarer inherited version. ADAMTS 13 being the disease common factor. Many aHUS patients will have been misdiagnosed with TTP so have experience of being a “TTP patient” TTP now has a drug treatment called Caplacizumab , though it will not help misdiagnosed aHUS patients. The heredity version of the disease has a different treatment in which defective ADAMTS13 is replaced. Again of no benefit to misdiagnosed aHUS patients who would already have enough ADAMTS13.
The sixth TMA illustrated used to be called HUS but now is called STEC-Associated Hemolytic Uremic Syndrome. This TMA is brought on by shiga toxin producing E.Coli and not Complement. But it can activate Complement and its membrane attack complex. It is possible that those predisposed to aHUS can onset after HUS trigger. aHUS patients frequently are diagnosed as having HUS. Eculizumab has uncertain benefits for true HUS patients.
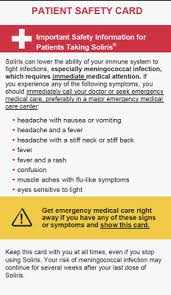
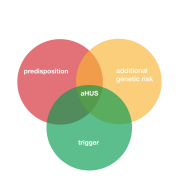
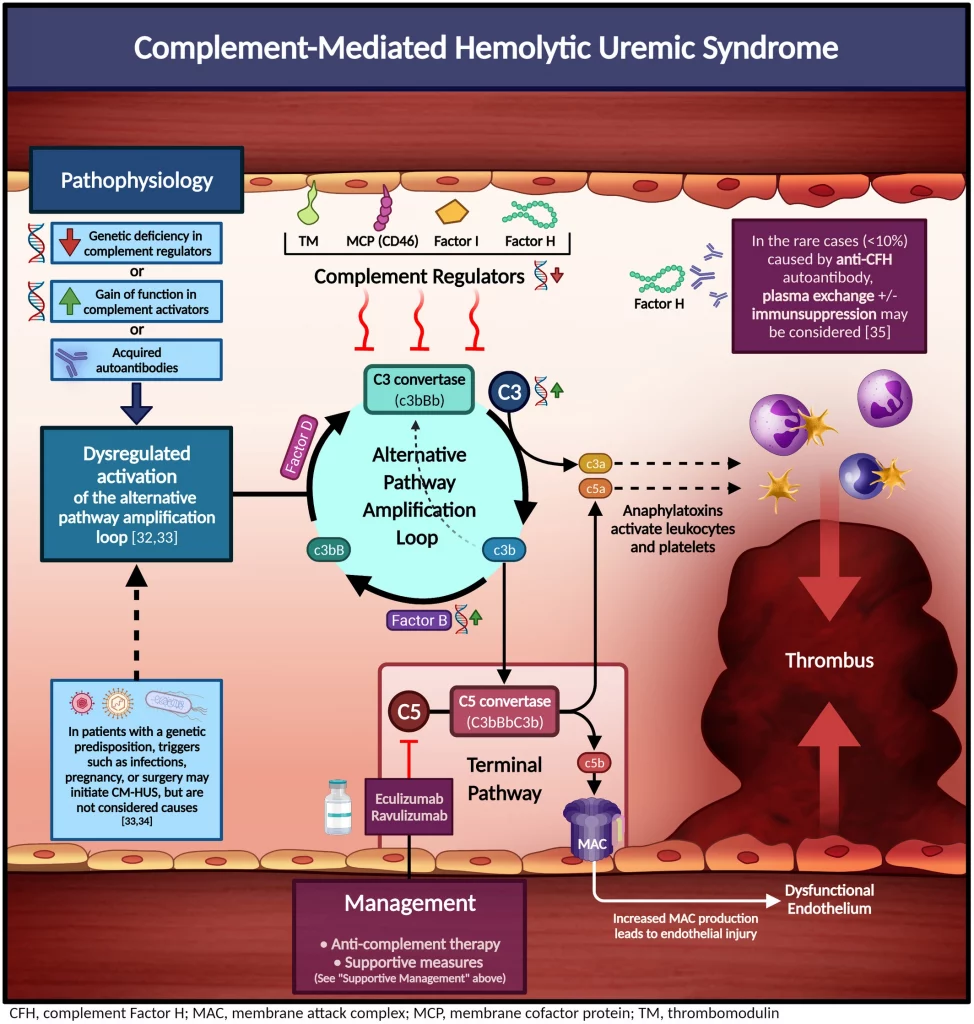
And then it is the turn of Complement -Mediated Hemolytic Uremic Syndrome. The Complement-Mediated Hemolytic Uremic Syndrome’s, which we know as aHUS’, illustration ( see above) should be very familiar to aHUS folk.Caused by dysregulation of the Complement system, due to no, or hampered, control, excessive activation that cannot be controlled and begins to injure endothelium in blood vessels which brings on a TMA.
Next comes Hematopoietic Cell Transplant- Associate Thrombotic Microgiopathy. Bone marrow transplant can cause TMA in some patients and short term blocking of Complement can help.
Drug -Induced Thrombotic Microagiopathy can result from some drugs used to treat many conditions. Withdrawal of that specific drug treatment can resolve the TMA.
The final illustration shows to which part of the complement system’s pathways current treatment available or in trial are directed. For aHUS Iptacopan is directed at Complement Factor B, Narsolimab inhibits MASP 2 in the Lectin pathway. Eculizumab and Ravulizumab inhibits C5 and Crovalimab inhibits C5b6 to stop the membrane attack complex.
Well worth seeing go to link above . It is like viewing the slides from a presentation. Images can be worth a thousand words.
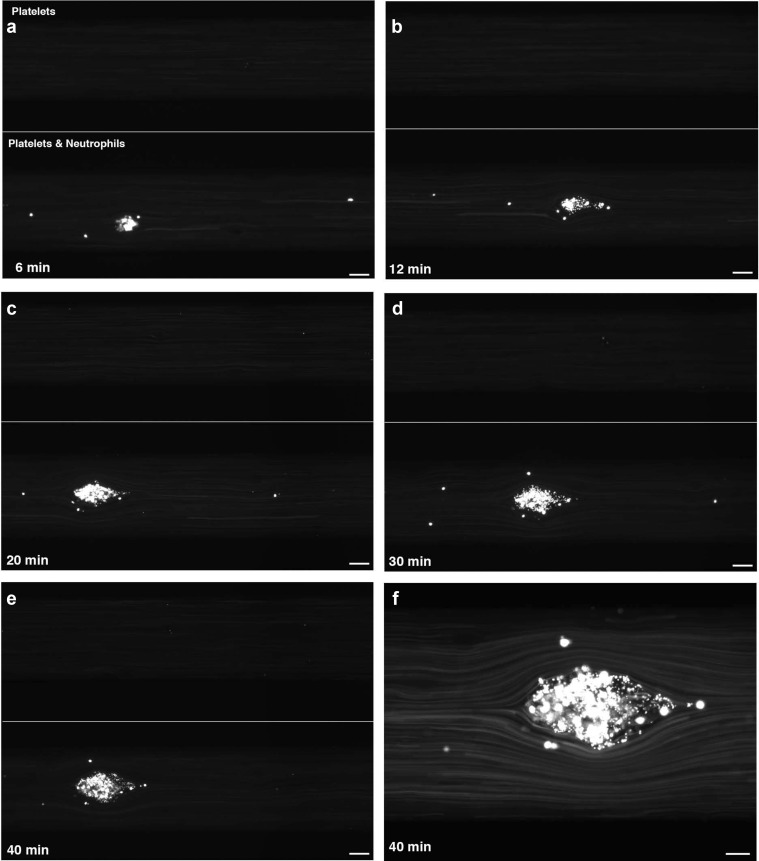
Here is another image this time from the Reidl Group which Global Action has featured before It is of an actual micro clot (TMA) forming on a damaged blood vessel and brought on by complement, platelets and neutrophils. In each case the top image has the same damaged blood vessel without them being present. When present at 6 minutes something happens…. At 40 mins look at how the blood is deviating and being squashed around the obstacle that has been formed. If more damage is created then more clots would make things worse and that is when blood cells start “exploding”.
It comes down to what causes the damage and which organ the blood vessels are feeding and how it would be affected. That determines which treatment would be the most effective. Helping that decision in future would be specific condition names to accurately diagnose the condition and properly direct the right treatment.
The aHUS clinical community is ready to redefine and drop the name aHUS. The acid test will be whether more rapid diagnoses in seven days or less result.
Article No. 528