Article No. 402
12 December 2020
Just over a year ago aHUS Global Action featured a series of articles “aHUS is its end really nigh?” about the renaming of aHUS. It finished off with an article about the classification of TMAs by Christoph Aigner and the TMA Group from Vienna, Austria. ( Article 303 )
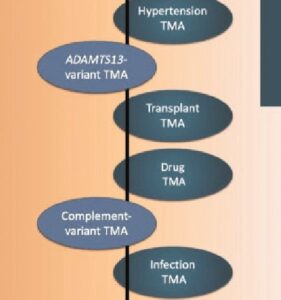
The Group had listed TMAs separately based on their cause, whether specific, generic or idiopathic and also the extent to which the diseases were inherited or acquired. An extract of the TMAs classification list can be seem above.
The classification triggered the question “who do aHUS patient groups advocate for?” when aHUS is not even specifically mentioned in the list of TMAs.
It was complicated . And the TMA nomenclatures have taken off to confuse patients and advocates.
A recent editorial in Nephrology Dialysis Transplantation NDT Journal of ERA/EDTA illustrates the difficulty. (click here to read full article)
Its title is “Malignant Hypertension and thrombotic microangipathy: complement as the usual suspect” and it has been written by Fadi Fakhouri and Veronique Freneaux-Bacchi, two aHUS researchers well known to us ,and a colleague of Fadi’s at Lausanne University Switzerland, Salina Sadallah.
It is about Malignant Hypertension ( MHT), which is a cause of renal disease. 1 in 20 MHT patients suffer with TMA too.
MHT is more common in aHUS. Between a third and half of aHUS patients have MHT.
aHUS is a complement mediated TMA.
The Fakhouri Group’s article sets out to “dissect the interconnect “ between the disorder through complement and TMA to aHUS. They do so by critiquing a contemporary research article by the Zhang Group about what it found in a study of 50 MHT patients.
Using urine analysis as well as plasma the Zhang Group found evidence of complement activation. The activation seemed to be just damaging the endolethial cells but not causing blood clots. They observed what is termed Malignant Nephrosclerosis.
The Zhang Group concluded “that dysregulation of the complement alternative pathway plays a role in the activity, severity and outcome of “malignant nephrosclerosis” and that screening for complement defects in patients with this disorder is warranted for the potential use of therapeutic complement blockade”
Although identifying limitations in the complement activation measures used in the study ,the Fakhouri Group found the interactions revealed between MHT TMA and aHUS of interest.
It raised the questions about whether MHT patients should be screened for complement genetic variants. And whether they would benefit from complement inhibition treatment transiently until the normal blood pressure is restored.
They also raised the point about what to call those MHT patients who could benefit from a complement inhibitor
Were they un-recognised aHUS patients , or Complement mediated nephrosclerosis patients , or even Hypertensive associated TMA patients?
Depends on whether complement is the “usual suspect or the culprit“.
Semantics here are important for diagnosis and for patients and it would be beneficial if there was a common language,according to the Fakouri Group.
Would someone with Hypertensive associated TMA be better treated if ,with another spin of the working diagnosis wheel, it became an aHUS diagnosis? Or is the HT-TMA an Eculizumab -TMA in its own right but not yet in scope?
If they are un-diagnosed aHUS patients we should be advocating for them. If not , who should?

