Article No. 374
3 September 2020
For most aHUS patients a diagnosis of aHUS was hard to come by. For a small number they may still not know what they had.
Diagnosis is a process that starts when an illness begins and symptoms begin to appear. Sufferers may initially make their own judgements of what is wrong with them. But when symptoms persist or get worse it is normal to seek expert medical advice to get a diagnosis and a treatment.
But diagnosing aHUS is a challenge.
It is a rare disease which most medics will never come across in their careers. It is also a Thrombotic Microangiopathy, a TMA.
aHUS , like TTP, is a Primary TMA but together they are a very small number of all TMAs.
Secondary TMAs ,as other TMAs are called , occur much more frequently that Primary TMAs.
Secondary TMAs include:
Shiga Toxin/HUS – more common than aHUS
Pregnancy TMA- a common trigger of TMA, ( most frequently due to HELLP)
Autoimmune disease TMA – rare trigger of TMA
Malignant Hypertension TMA– rarely happens ,like aHUS
Malignancy TMA– triggers more TMAs than you would think
Monoclonal Gammopathy of Unknown Significance TMA- a rare event
Infection TMA- adds a lot more TMAs than Shiga Toxin and E.coli alone , COVID19 may add to them
Transplant TMA– a not infrequent TMA occurrence
Drugs TMA– a common trigger
Other TMA – includes sickle cell disease, Vitamin B12 deficiency, Glucose 6 phosphate deficiency, Folate deficiency and even large haematomas.
TMAs are common enough for more doctors to be aware of it. But how common?
There is a very little detailed information about the incidence of TMAs. Even less about how numbers are spread over Primary and Secondary types of TMA.
Some insight, however has been given by an article published last year “Etiology and Outcomes of Thrombotic Microangiopathies” . (Click HERE to read the full article).
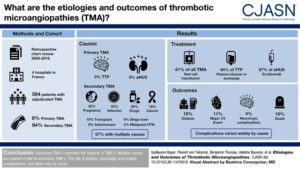
Pictorial abstract from Bayer et al article
Led by Guilliaume Bayer, some researchers from France looked at over 1600 records of patients admitted to four hospitals in Tours area ( population 1 million) with a clinical symptom that would be seen in someone with a TMA. After excluding those who did not meet the full criteria and examining individual records the researchers concluded that 564 patients in the years 2009 to 2016 had a TMA diagnosis.
The research group then broke down the TMAs into their sub types and provided key characteristic and clinical data about each. The full analysis can be seen in Table 2 of the article. the following table shows the relative numbers/ percentages of each primary TMA and all Secondary TMAs.
| No, of incidents in 2009 to 2016 | % | Incidence Rate per million | |
| aHUS | 15 | 3 | 1.9 |
| TTP | 18 | 3 | 2.3 |
| All secondary TMAs | 531 | 94 | 66.0 |
| Total TMAs | 564 | 100 | 70.0 |
If this is representative then for every 100 patients presenting with a TMA only would 3 patients will get a diagnosis of aHUS diagnosis, Demonstrating the challenge of an aHUS diagnosis.
In a country like the USA if the 70 per million incident rate for TMA is applied , it would mean more than 600 patients with aHUS out of an overall incidence of 22000 TMAs could present each year.
There is probably a prevalent population of over 200,000 people who have been affected by a TMA. At that level TMAs would not be a rare diseases but ultra rare aHUS would be among them.
Quite a challenge for aHUS.
However the Study results show relatively low TTP numbers and the aHUS numbers seem very high relative to TTP .
If the aHUS incidence is around 1 per million of the population say and the overall TMA incidence rate is about right , doctors would be expected to spot around about 300 patients per year, 6 new patients per week on average , throughout the country.
A bigger challenge.
All aHUS patients have a diagnosis story to tell. It would be interesting to see what the common issues and themes of the collective journey might reveal.
Maybe that would help aHUS patients yet to onset. Today they are very unlikely to be aware of aHUS at all.
aHUS Awareness Day is 24 September 2020.

