Article No. 320
19 February 2020
Continuing in the series of news blogs about Ravulizumab, which so far has covered dosing, special patient groups and developments, here the spotlight is on the key side effects from using the drug.
Risk of serious meningococcal infections – as was the case with eculizumab life threatening meningococcal/sepsis has occurred in patients prescribed Ravulizumab and the same precautions are mandated. Patients should be immunised at least 2 weeks before the first infusion in accordance with advisory practices, unless the risk of delaying immunisation outweighs the risk of becoming infected. Patients should be closely monitored for signs of infection.
So hence the important advisory notice-
WARNING: SERIOUS MENINGOCOCCAL INFECTION
Patients treated with Ravulizumab, like those treated with eculizumab, need to be vigilent in complying with vaccination and prophylactic use of antibiotics when prescribed. Revaccination is required according to guidelines
Whilst precautions cannot eliminate the risk of breakthrough meningococcal infection they can help minimise the long term effects once treated
These are the signs and symptoms of meningococcal infection/sepsis, and patients are advised to seek immediate medical attention if these signs orsymptoms occur.
• headache with nausea or vomiting
• headache and a fever
• headache with a stiff neck or stiff back
• fever
• fever and a rash
• confusion
• muscle aches with flu-like symptoms
• eyes sensitive to light
Patients are to be given a Patient Safety Card that they should carry with them at all times. This card describes symptoms which, if experienced, should prompt the patient to immediately
seek medical evaluation
Other infections -as well as “neisseria meningitidis” those treated with Ravulizumab are at risk of other encapsulated bacterial infections including “streptococcus pneumoniae”. Children may be at increased risk of that and “haemophilus influenzas”. To a lesser extent infection in adults by “neisseria gonorrhoeae” is another risk from Complement inhibition.
Preventative vaccinations for streptococcus pneumonia and influenzae can minimise those risk.
Monitoring of active infections is a must do.
Discontinuation– Ravulizumab treatment should be continued for a minimum of six months, but after 6 months treatment should be individualised based on patient specific risk factors. So a case of when needed for as long as is needed( Minimum 6 months) . It is not for life for everyone but neither is withdrawal for everyone. This is a significant change in prescription advice from eculizumab.
The patient risk factors to be taken into account are the genetic susceptibility to aHUS and the longevity of the triggering event. Much as the alliance tried to convey in its “relapse risk matrix”.
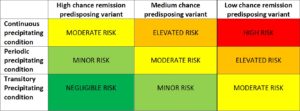
The relative factors need to be populated with specific mutations/variants and triggering events based on research evidence. This could result in a “prognosis algorythm” which could be used by doctors everywhere to guide their withdrawal decisions for their aHUS patient based on the wider research evidence.
No data as has been collected yet for ravulizumab as has been gathered about eculizumab withdrawal, but it is advised that patient monitoring should be conducted for at least 12 months; watching for signs of “seizures, angina, dyspnea, thrombosis, high blood pressure and mental state”. Blood measures including platelets, creatinine and LDH levels should be tested for increases on levels measured whilst on Ravulizumab treatment. For eculizumab withdrawal self monitoring urine dips have been used to good effect.
If there are signs of aHUS recurrence then reinitiating Ravulizumab should be considered.
Infusion Reactions– reaction to an infusion can incur. In clinical trials, 5 out of 296 ( 222 PNH, 74 aHUS) patients treated with ravulizumab experienced infusion reactions including lower back pain, drop in blood pressure, infusion-related pain, elevation in blood pressure and limb discomfort during its administration. They did not mean that Ravulizumab was discontinued. If signs of cardiovascular instability or respiratory compromise occur then infusion will be interrupted.
Adverse events – comparison of adverse events reported during the aHUS trial for ravulizumab cannot be made with the eculizumab trial reported outcomes. Adults(n=58) in the ravulizumab trial reported 277 adverse events across a range of conditions e.g, headaches, diarrhoea, hypertension, anxiety, whilst children ( n=15) reported 65.
The most frequent serious adverse actions reported in more than 2 patients (2.7%) treated with ravulizumab were hypertension, pneumonia and abdominal pain.
Four patients died during the ALXN1210-aHUS-311 study. The cause of death was sepsis in
two patients and intracranial hemorrhage in one patient. The fourth patient, who was excluded from the trial after a diagnosis of STEC-HUS, died due to pretreatment cerebral arterial thrombosis
Fuller highlights about the prescription of ravaulzumab can be read here.

