Skin is considered the largest organ of the human body, accounting for about 15% of the body’s weight and covering an area of approximately 2 square meters (21 sq ft) for the average person. Medical literature includes some case histories of atypical HUS patients with skin issues, and research indicates that aHUS may be diagnosed by skin biopsy. Here the aHUS Alliance has compiled information and sourced medical literature regarding the related topics of skin biopsies to diagnose atypical HUS and of potential for people with atypical HUS to have skin involvement as an extra renal manifestation of aHUS.
On average the human body has 300 million skin cells and the skin renews itself every 28 days to replace dead cells, which are shed on average at a rate of 30,000 to 40,000 cells per minute. (Click for more skin facts) While the liver is the body’s largest internal organ, the skin is considered an organ (rather than classified as a tissue) since skin is a group of specialized cells that fill specific functions such as maintaining body temperature and protecting the other organs. The skin includes epithelial, nerve, vascular, and connective tissues, with changes in skin sometimes acting to signal changes in health. Why is the atypical HUS interested in learning more about skin issues and becoming aware of potential aHUS impact?
In 2015, research published by Magro C et al noted that “skin biopsy is of value in establishing a diagnosis of aHUS even in the absence of clinically discernible skin lesions.” Some atypical HUS patients may experience skin issues related to disease activity, with Hofer et al noting that “skin involvement is a rare but maybe under diagnosed complication in the context of complement-mediated TMA and is reported for three patients in the literature”, mentioning the 2014 work of Ardissino et al that Hofer described as, “three cases of complement-mediated aHUS, two with a CFH mutation and one with CFH-Ab HUS, who developed skin lesions that completely recovered after establishing PT or eculizumab.” To provide context, connections, and clarity, we provide a brief overview of terms prior to listing excerpts from various medical journals on the topic of aHUS, TMA, and skin involvement. The aHUS Alliance offers information to aid awareness of this very rare disease, to encourage others to launch ‘deep dives’ and create atypical HUS resources, and to foster insight into the need for more collaboration and aHUS research.
The following is only a small segment of current information available, with recognition that much further study and research needed into atypical HUS. Only a patient’s medical team can determine appropriate care plans for their situation, and we encourage those with questions about aHUS and potential skin issues to contact their physicians.
Note: The aHUS Alliance appreciates the kindness of Dr. Gianluigi Ardissino in granting permission to post the full text version of the article Skin involvement in atypical hemolytic uremic syndrome (Ardissino G et al, 2014) in our website’s Info Centre within the Publication section. Thank you!
Glossary of Select Terms
Extra renal manifestation – Atypical HUS can impact organs other than the kidneys. “Extra renal” refers to organs and body systems other than kidneys such as heart, brain & nervous system, lungs, eyes, GI tract, skin, and other parts of the body. The term “manifestation” refers to the occurrence or involvement of other organs, appearing to affect parts of the body. (See more: Extra-Renal Manifestations of Complement-Mediated Thrombotic Microangiopathies Hofer et al, 2014)
Thrombotic Microangiopathy (TMA) – A main characteristic of atypical HUS is the formation of tiny blood clots that systemically can occur throughout the body, known as ‘thrombotic microangiopathy’ (TMA). Raised lining of the small vessels and clots blocking them can shear red blood cells into pieces, which impacts their ability to carry oxygen from the lungs throughout the body. Patients with aHUS often have compromised kidney function due to TMA damage, although an estimated 20% of aHUS patients present with preserved renal function at diagnosis. Patients with atypical HUS often have many of these symptoms: blood and blood vessels are affected, red blood cell counts are low (anemia), platelet counts drop (used in clotting, thrombocytopenia is too few platelets) and tiny clots which may form anywhere in the body but often affect the kidneys and brain. Development of tiny clots (thrombi) can happen in different parts of the body to cause sudden or life-threatening conditions such as seizures, vision loss, stroke, cardiac issues, kidney failure and other serious medical situations. (See more: Is it aHUS? Perhaps it’s TTP, STEC-HUS, or Another TMA) aHUS Alliance, Burke 2017)
skin biopsy – Medical procedure in which a sample of skin tissue is removed, for examination and testing in a laboratory
cutaneous – referring to or related to the skin
lesions – from the Latin word ‘laesio’ meaning injury. There are many types of lesions, referring to a region with damage or tissue change most often caused by disease or trauma (such as a wound, ulcer, abcess, tumor etc)
cutaneous ulcer – a sore on the skin, accompanied by the disintegration of tissue which may be caused by an inflammatory cause or microvascular issue
microvasculature – smallest blood vessels, from ‘micro’ meaning small and ‘vasculature’ referring to blood vessels
gangrene – tissue death and decay in a living organism, usually a limb or digit (finger, toe) caused by a critical lack of blood flow as a result of injury, infection, or disease.
necrosis – death or microscopic injury to cells. Necrosis pertains to premature death at a cell level, whereas gangrene is a type of necrosis on a large scale that involves a mass death of body tissues.
sepsis – a large scale immune response to bacterial infection in the blood stream, which can lead to life-threatening organ dysfunction, or organ injury and failure. Toxins related to bacterial infections which tissue death and decay could become a causal factor for sepsis.
endothelial injury – damage to the single cell layer of tissues that lines all blood vessels, whose main function includes the tasks which regulate exchanges between the bloodstream and the surrounding tissues
ischemic changes – Ischemia an inadequate blood supply to an or organ or part of the body, and is generally caused by a blood vessel problem that restricts blood supply to tissues. If there is a shortage of oxygen and glucose needed to maintain cell metabolism (keeping tissue alive), damage or tissue dysfunction/death can occur.
Petechiae (puh-TEE-kee-ee)
Petechiae are tiny spots in the skin which may appear as purple, red, or brown spots in the mucous membranes (mouth or eyelids) or skin locations on the arms, legs, stomach, or buttocks or less commonly on the face, neck, or chest. Grouped in clusters petechiae may look like a rash, but are usually flat rather than raised or bumpy and unlike a rash when pressed these dots of petechiae do not lose their color. They are not itchy or painful. As a sign of blood leaking from capillaries under the skin, petechiae are a symptom (rather than a disease). Petechiae may be caused by an infection, medication, or illness and is known to occur in certain blood disorders (to include aHUS). Check with your doctor if you’re concerned about spots on your skin, since some conditions causing petechiae may be serious and indicate need for medical care. Click here FMI
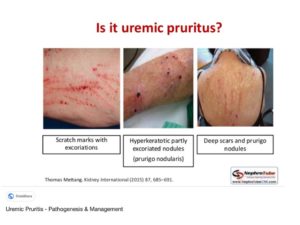
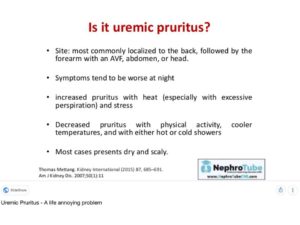
Uremic Pruritus (also known as ‘Renal Itch’)
As implied by the ‘uremic’ part of its name, uremic pruritus occurs due to excessive urea in the blood due to chronic kidney disease or when the kidneys stop working (renal failure). Originating from the Latin prūrītus (“itch, itching”) and borrowed from prūriō, pruritus is the medical term for itchy skin. Sometimes known as chronic kidney disease-associated pruritus (CKD-associated pruritus), this condition is common with dialysis patients.According to DermNet.org: “The prevalence rates of uremic pruritus are between 20–50% in those with chronic kidney disease, however, the reported rates appear lower in children at approximately 9%. Uraemic pruritus is not associated with sex, age, ethnicity, duration of dialysis, or cause of renal failure.” If you have itchy skin and have a chronic kidney disease like aHUS, consult with your doctor both to ask about itch relief options and to review your current medical status and kidney health.
Medical Literature – A Curated Review
of Articles regarding aHUS & Skin Issues
The Role of the Skin Biopsy in the Diagnosis of Atypical Hemolytic Uremic Syndrome (Magro, C et al)
“The skin biopsy has potential to play a very important role in the diagnosis of aHUS.”
In the majority of cases in this study, the biopsies were of normal skin from the forearm or deltoid. In one patient, a biopsy was only performed from the toe ulcer and in another patient biopsies were taken from both the normal deltoid skin and a toe ulcer. In two patients, biopsies were performed only on the lower extremity. Two patients had a biopsy of normal abdominal skin. We recommend the deltoid area…”
“A number of biopsies were performed on patients who had symptoms encountered in aHUS but had other reasons such as systemic lupus erythematous, HELLP, and TTP as the etiologic basis of the multiorgan thrombotic diathesis and or hemolysis and or did not have enough symptoms and abnormal lab findings to render a diagnosis of aHUS.”
“Biopsies of skin were procured from nine patients with HUS. Eight of these patients had diagnostic features of aHUS while one patient had Escherichia (E) coli triggered HUS. In addition, thirteen biopsies were obtained from patients who did not fulfill diagnostic clinical criteria of atypical HUS.”
“5 women and 4 men from 25 years to 71 years of age (mean age of 46 years) comprised the 9 patients of the study group. One patient had classic E. coli triggered HUS. Clinical features common to all 9 patients included renal insufficiency, abnormalities in liver function tests, hemolysis, and thrombocytopenia. Among underlying medical conditions were myelofibrosis, colonic adenocarcinoma, membranous glomerulonephritis, idiopathic pancreatitis, sepsis in the setting of chorioaamnionitis and sepsis induced by retention of products of conception.”
“In two patients from the cohort, both females, cutaneous lesions were observed on examination. One patient, a 24-year-old women presented with sepsis and DIC secondary to chorioamnionitis in the 16th week of pregnancy. She was found to have retiform purpura on the left 4th toe. The other patient had cutaneous ulcers of the second toe.”
“In two patients from the cohort, both females, cutaneous lesions were observed on examination. One patient, a 24-year-old women presented with sepsis and DIC secondary to chorioamnionitis in the 16th week of pregnancy. She was found to have retiform purpura on the left 4th toe. The other patient had cutaneous ulcers of the second toe.”
Skin involvement in atypical hemolytic uremic syndrome (Ardissino G et al, 2014)
“Skin involvement in atypical hemolytic uremic syndrome (aHUS) is very uncommon and therefore often unrecognized as a specific symptom of aHUS. We describe 3 cases of patients with aHUS who developed skin lesions that completely recovered when disease-specific treatment was established. These cases suggest that in individuals with aHUS, when skin lesions of unknown origin occur, the possibility that they are due to thrombotic microangiopathy should be considered.”
“In conclusion, we describe what to our knowledge are the first cases of skin involvement associated with (and possibly caused by) CFH-associated aHUS and encourage physicians caring for patients with aHUS to consider any skin lesions of unknown origin as possible manifestations of TMA, although the TMA may not be fully evident in laboratory tests.”
A rare case of cutaneous involvement in atypical haemolytic uraemic syndrome successfully treated with eculizumab (Lopes D et al, 2016)
“A 35‑year‑old female presented to our hospital with painful skin lesions. Her past medical history included: one uneventful pregnancy and a second pregnancy complicated by pre‑eclampsia and C‑section performed at the 29th week of gestation; chronic kidney disease (CKD) on haemodialysis due to aHUS, diagnosed after her second pregnancy. A few months after childbirth, she presented with severe hypertension and oedema and the workup performed showed microangiopathic haemolytic anaemia, thrombocytopoenia and acute kidney injury possibly triggered by pregnancy or respiratory infection.”
“Extra‑renal TMA manifestations are observed in up to 20% of patients, including involvement of the central nervous system, cardiovascular system, lungs, skin, skeletal muscle, and gastrointestinal tract. As previously reviewed those extra‑renal complications may not only be observed during the disease’s acute phase but can also manifest to some degree years later and are thought to result from a chronic over activation/dysregulation of the complement system. Affected patients have a lifelong risk of systemic clinical complications of TMA.”
“In the patient reported here, we noted perfusion defects of arterioles supplying the skin, leading to gangrenous and ulcer lesions that appeared before the haemolysis parameters. Gangrenous lesions of the finger and toes were reported in six children with aHUS in three case reports.”
An Atypical Case of Atypical Hemolytic Uremic Syndrome: Predominant Gastrointestinal Involvement, Intact Renal Function, and C5b-9 Deposition in Colon and Skin (De Yao J. et al, 2015)
“We report a unique case of aHUS in a 71-year-old female highlighted by predominant effect on the gastrointestinal system concurrent with preservation of renal function and histopathologically-proven involvement of skin.”
“Atypical hemolytic uremic syndrome (aHUS) is a previously under-recognized form of TMA which, in the majority of cases is a consequence of a genetically based dysregulation of the alternate complement pathway (AP). Microangiopathy in aHUS is the end-organ effect of a systemic complement-mediated diathesis which has the propensity to affect the vascular bed of all organs but exhibits a particular affinity for the renal, central nervous, and gastrointestinal systems (in this order of frequency). Historically, the majority of reported cases have included some degree of renal dysfunction, frequently including end-stage renal disease. Skin involvement is not a commonly reported finding, but both clinically apparent and sub-clinical involvements have been described in some recent publications. We describe, herein, a unique case of aHUS highlighted by recurrent pancreatitis, ischemic colitis, and preserved renal function, with pathological assessment demonstrating microvascular thrombosis and endothelial complement deposition in colon and skin.”
“Without apparent kidney dysfunction, histological evidence of non-renal, TMA-related organ involvement was sought.”
“Punch biopsies were performed on normal skin based on previous reports of potentially diagnostically useful information being gleaned from histopathological evaluation of cutaneous vessels. Our biopsy results were interpreted as endothelial injury in the presence of platelet/fibrin microthrombi consistent with TMA.”
Peripheral gangrene complicating idiopathic and recessive hemolytic uremic syndromes (Kaplan BS et al, 2000)
“Three patients with hemolytic uremic syndrome (HUS) developed peripheral gangrene. Bilateral carotid artery thromboses occurred in one of these patients after recovery from HUS. One patient had a long history of juvenile rheumatoid arthritis. In the second patient, a flu-like illness preceded the onset of HUS. The third was one of two sisters, with the HUS appearing more than 1 year apart. None had evidence of disseminated intravascular coagulation or infection with Streptococcus pneumoniae. The patient with rheumatoid arthritis had renal cortical necrosis but recovered moderate renal function after treatment with dialysis and plasmapheresis for 6 months. The child with a genetic form of HUS died of renal failure and had massive cortical necrosis and vascular thrombosis at autopsy. This is the first report of peripheral gangrene in children with idiopathic HUS and autosomal recessive HUS.”
Peripheral gangrene complicating hemolytic uremic syndrome in a child (Özel A. et al, 2003)
“A patient with hemolytic uremic syndrome (HUS) developed peripheral gangrene involving all fingers and toes.” and “All medial and distal phalanxes became necrotic and were removed surgically”.
Digital gangrene in a child with atypical hemolytic uremic syndrome associated with anti-factor H antibodies (Sathe K.P. et al, 2016)
“Our patient presented with HUS-TMA with anti-factor H antibodies. Anti-Factor H antibodies result in uncontrolled complement activation and have emerged as a major cause of HUS in the Indian subcontinent. Although HUS can have extrarenal involvement in one-third of the cases, peripheral gangrene is extremely rare as the size of the vessels supplying the digits is relatively much larger than the microvasculature commonly affected in HUS. Comorbid infections, vasculitis or prothrombotic disorders that can lead to digital gangrene were ruled out. The digital gangrene was thus attributed to persistent HUS activity. Eculizumab, a C5 blocking antibody that has been found effective in salvaging such cases, could not be offered due to unaffordability.”
Cutaneous involvement in haemolytic uraemic syndrome. (Santos C. et al, 2013)
“Although being extremely rare, we should be mindful of skin involvement in aHUS and establish this association in a timely manner which would lead to an early diagnosis and correct treatment, avoiding wasted time and costs.”

Related Readings: More about Skin Issues
ESRD and Dialysis
Dermatologic Manifestations of End-Stage Renal Disease (Brewster U, 2006)
Skin changes in dialysis patients: a review (Avermaete A et al, 2001)
Comparison of uremic pruritus between patients undergoing hemodialysis and peritoneal dialysis (Min J et al, 2016)
Complement System and Skin
Complement System in Dermatological Diseases – Fire Under the Skin (Panelius J and Meri S, 2015)
Kidney Disease and Skin Issues
Dermatological diseases in patients with chronic kidney disease (Gagnon A and Desai T, 2013)
Renal Disease and Skin Problems (Fields D, 2016)
D Fields – “Pruritus or itching: One of the most common skin conditions related to renal disease is pruritus, or severe skin itching. About 50-90% of patents on dialysis experience pruritus, while around 15-49% of patients who have chronic kidney disease acquire the condition.”
Dermatologic Manifestations of Renal Disease (Nunley J, 2016)
J Nunley – “ …other primary dermatologic manifestations associated with uremia including the following:
Xerosis
Pruritus
Pigmentary alteration
Half-and-half nails
Alopecia
Uremic frost
Porphyria cutanea tarda
Arterial steal syndrome”

Uremic Pruritus (Mettang T and Kremer A, 2015)