The topic of pregnancy and aHUS is included in the Global aHUS Patients’ Research Agenda. It has featured in articles on this website. It has been a subject of interest to this author since involvement in a health policy decision about using eculizumab for aHUS.
Back then there was little information on the topic. What existed was mostly related to eculizumab use for pregnant PNH patients.
Over the past five years much more is now known. It is advised that women with aHUS can chose to to get pregnant and any eculizumab treatment does not harm the unborn child.
But families differ.
In those women who may have had aHUS and are currently being treated with eculizumab their decisions would be based on different information to those who are now in remission from aHUS and have withdrawn from treatment. In the latter instance it is the likelihood of recurrence of aHUS during pregnancy or even post partum which is important to them and how quickly eculizumab can be accessed if needed , and for how long it will be needed.
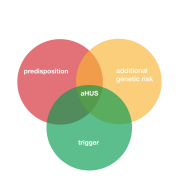
Those women who have never had aHUS but have tested positive for an aHUS predisposing genetic factor are in a similar situation as those who have not been tested but are closely related to a family member who has had aHUS. Particularly if that aHUS has been triggered by pregnancy.
What happened to the three sisters from Missouri is a cautionary tale.
It is a case study ( and story ) about the pregnancies of three Hispanic sisters from Missouri reported on at ASN 2019.
Each of the sisters experienced post-partum symptoms within 7,7 and 10 days of their deliveries in 2006 , 2014 and 2015 at ages of 18, 24 and 25 respectively.
The first and second sister had identical symptoms of anaemia , thrombocytopenia and acute kidney injury but did not get an aHUS diagnosis, even though the first sister’s kidney biopsy had revealed evidence of TMA.
The third sister also had a kidney biopsy showing evidence of TMA and was diagnosed with aHUS and treated with PEX and dialysis until she experienced acute heart failure and was treated with Eculizumab, and within two weeks she had recovered.
The first sister had also experienced acute heart failure and recovered. The second sister was then diagnosed as having aHUS given eculizumab and then after two years stopped dialysis.
Genetic testing was undertaken and each sister had multiple variants/mutations in their Complement factors H , I and MCP. The multiple genetic variants had increased the risk of onset.
Where did the mutations come from as there is no mention of the sister’s mother having experienced difficulties in pregnancy? The researchers do however reveal that their father’s mother had lost 10 out of 12 pregnancies!
Family history of pregnancy problems involving renal failure adds to the information needed to make a decision.
That leaves one group of women. They cannot be informed ahead of their encounter with aHUS , not even as a potential complication of pregnancy. Most aHUS onsets happen post partum and so does not impact on the unborn child.
During pregnancy a thrombotic microangipathy is a rare occurrence ( 1 in 20,000 pregnancies ) and it is even more rare that aHUS is the cause ( 1 in 2 million pregnancies?) .
If diagnosed quickly and eculizumab is administered a full term pregnancy is possible with a successful outcome and with no damage from eculizumab.
If not diagnosed but an unborn child could survive , an induced delivery can usually stop the TMA in the parent, but if the TMA is aHUS, eculizumab treatment will probably still be needed.
If the foetus is not viable for delivery, a termination of the pregnancy can be performed. Or it is possible a sporadic abortion may occur But eculizumab is still likely to be needed by the mother. More aHUS pregnancies are terminated than PNH pregnancies both of which have eculizumab as the common treatment. Decision making timelines may differ.
Getting information to those parents in trying circumstances and uncertain treatment access, and in time to make an informed decision, remains the challenge to save unborn aHUS babies.
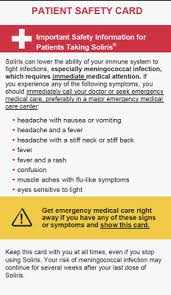
For all parents the issue of what effect eculizumab has on the unborn child or from milk from breast feeding is important.
The research agenda question is “Do aHUS families have all the correct information to make informed family planning decisions?”. In 2021 it would appear that there is plenty of information from research into aHUS pregnancy and use of eculizumab ( and thus ravulizumab) to inform parents.
The issue is whether there is awareness of it and it is assembled in such a way to be readily available for all stakeholders when a decision needs to be made, particularly if that decision is urgent .
As always comments and questions about these articles are welcome in the comments box at the bottom of the page. If any viewer of this article is aware of any issue about aHUS pregnancy that has not been answered yet please let us know.
Article No. 462
(A small selection from the 57 articles found in the search referred to above are cited below to illustrate different perspectives of this topic)
Gäckler A, Schönermarck U, Dobronravov V, La Manna G, Denker A, Liu P, Vinogradova M, Yoon SS, Praga M. Efficacy and safety of the long-acting C5 inhibitor ravulizumab in patients with atypical hemolytic uremic syndrome triggered by pregnancy: a subgroup analysis. BMC Nephrol. 2021 Jan 6;22(1):5. doi: 10.1186/s12882-020-02190-0. Erratum in: BMC Nephrol. 2021 Feb 2;22(1):49. PMID: 33407224; PMCID: PMC7786907.
Puri P, Hanxhiu A, O’Hara DV, Hsu D, Vucak-Dzumhur M. A life-threatening case of pregnancy-related atypical Haemolytic uremic syndrome and successful treatment with Eculizumab. BMC Nephrol. 2020 Nov 17;21(1):488. doi: 10.1186/s12882-020-02100-4. PMID: 33203373; PMCID: PMC7670627.
Winchester ML, Platzbecker R, McMahon M, Parrish M. Eculizumab Maintenance and the Prevention of Atypical Hemolytic Uremic Syndrome Relapse During Pregnancy: A Case Report. J Med Cases. 2019 Dec;10(12):343-344. doi: 10.14740/jmc3397. Epub 2019 Dec 31. PMID: 34434305; PMCID: PMC8383567.
Fakhouri F, Scully M, Ardissino G, Al-Dakkak I, Miller B, Rondeau E. Pregnancy-triggered atypical hemolytic uremic syndrome (aHUS): a Global aHUS Registry analysis. J Nephrol. 2021 Apr 7. doi: 10.1007/s40620-021-01025-x. Epub ahead of print. PMID: 33826112.
Morales E, Galindo A, García L, Villalaín C, Alonso M, Gutiérrez E, Rodríguez-Almaraz ME, Praga M, Herraiz I. Eculizumab in Early-Stage Pregnancy. Kidney Int Rep. 2020 Oct 10;5(12):2383-2387. doi: 10.1016/j.ekir.2020.09.045. PMID: 33305137; PMCID: PMC7710878.
Kelly RJ, Höchsmann B, Szer J, Kulasekararaj A, de Guibert S, Röth A, Weitz IC, Armstrong E, Risitano AM, Patriquin CJ, Terriou L, Muus P, Hill A, Turner MP, Schrezenmeier H, Peffault de Latour R. Eculizumab in Pregnant Patients with Paroxysmal Nocturnal Hemoglobinuria. N Engl J Med. 2015 Sep 10;373(11):1032-9. doi: 10.1056/NEJMoa1502950. PMID: 26352814.
Sarno L, Tufano A, Maruotti GM, Martinelli P, Balletta MM, Russo D. Eculizumab in pregnancy: a narrative overview. J Nephrol. 2019 Feb;32(1):17-25. doi: 10.1007/s40620-018-0517-z. Epub 2018 Aug 29. PMID: 30159857.