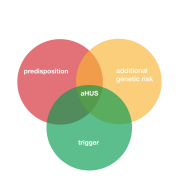
Take “diacylglycerol kinase ” and add a “syndrome” throw in a letter from the Greek alphabet ” ε” and you have the makings of the name of a rare disease- diacylglycerol kinase ε syndrome and like many rare diseases unpronounceable, so shorten it to DGKε Syndrome. Then have a different abbreviation and it becomes DGKE Syndrome. Except those with a DGKE problem already have two disease names. Nephrotic Syndrome and aHUS.
A defect in DGKE is a cause of a TMA with “aHUS like” symptoms and was discovered within the last 10 years. Prior to that it would have been just another idiopathic case of aHUS.
The striking thing about the discovery of DGKE was that the mutation that predisposes someone to a TMA was not found in a Complement component but in the lining of the endothelial cells. DGKE role was to protect the linings of the capillaries from clotting by the coagulation system and not to control a Complement attack.
Faulty DGKE exposes the capillaries to clotting and those clots result in red blood cells destruction by shear stress and can lead to kidney failure, If that sounds familiar it is because it what happens in aHUS too.
But DGKE patients are different to aHUS patients. There are very few of them. Estimates of incidence of a DGKE generated TMA are about 0.009 per million population if applied worldwide it would mean about 70 patients present with it each year, among the 4000 or so (0.5 per million) aHUS patients on-setting.
aHUS is an ultra rare disease but DGKE really is so much ULTRA RARER.
DGKE patients are very young. Half present before 9 months old and nearly all by 2 years old. 50% of patients need dialysis but mostly for only three weeks or so.
After management all recover and go into remission with some relapse incidents, which taper off after 5 years and rarely occur after 8 years. Most will have a legacy of varying stages kidney diseases and for a minority end stage renal failure can happen but it takes a long time to develop. Kidney transplants can be successful and they are not the trigger they are for HUS patients. Indeed triggers of DGKE TMA are rarely identifiable. Infections can set things off ( like for aHUS) and in some patients there are coexisting development disorders ( growth delay. learning difficulties or autism) . Growing up may bring it on, and there is evidence that patients can grow out of it happening again.
aHUS TMA caused by complement dysregulation insulting the endothelium can be treated with a complement inhibitor to stop Complement “insults”, but DGKE endothelial damage is caused by itself inviting the coagulation system to do its worst.
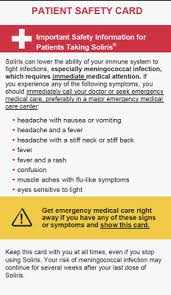
The consensus has been that complement inhibitors like eculizumab do not work for DGKE TMAs. Although researchers admit that how DGKE causes a TMA is poorly understood. In a study by the Brocklebank group of a small cohort of 16 international DGKE aHUS/ Nephrotic Syndrome patients , successful withdrawal of eculizumab due to non response by patients was the conclusion ( see full article HERE)
So we know DGKE disease patients have an aHUS like illness, It is caused by TMA. It has a lesser morbidity than aHUS but it does not have a specific treatment.
DKGE is also implicated in Nephrotic Syndrome . Although there are several causes of NS, Membranous nephropathy is one and is a kidney disorder resulting from thickening membranes within the glomeruli. The thickening is due to deposits made by the immune system. It can be associated with other medical conditions, such as lupus, hepatitis B, malaria and cancer, or it can occur for no known reason, One reason not mentioned is a DGKE mutation. Not surprising.
DGKE is an ultra rare disease much rarer than the collective aHUS cohort, 70 and 4000 incident patients respectively estimated worldwide annually. Nephrotic Syndrome incidence is 20 to 70 per million or between 156,000 and 546,000. Membranous Nephropathy patients incidence is less, 8 to 10 per million, roughly 62,400 to 78,000 patients annually. MPGN incidence is nearer aHUS and DGKE patients are almost as likely to have MPGN like clinical symptoms as they are of having aHUS.
aHUS is going through a name change process. DGKE disease is only aHUS like. In its analysis of Chrisoph Aiger Group classification of TMAs ( click HERE) this is what Global Action thought of where DGKE mutation patients rested on any reclassification.
DGKE variant:
” DGKE plays a part in controlling the coagulation system and clotting. When it does not function as it should, a prothrombotic state can follow which can lead to TMA. It is not a part of Complement and not treatable with eculizumab but it has been regarded as an aHUS. Inclusion in “new aHUS” is as open as it is for MMACHC TMA.“
Nephrotic Syndrome and MPGN patient organisations are unlikely to be concerned about DGKE as they have such big numbers to advocate for that a cohort of 70 people will hardly register among tens or hundreds of thousands.
Although the scale is less aHUS patient organisations have not necessarily advocated for DGKE patients; neither raising awareness nor concern about an apparent unmet medical need. A specific treatment for DGKE TMA presents a challenge. Firstly, in there being clinical trials and then if something clinically effective is discovered how high a price will it be, Complement inhibitors for aHUS cost more than $500,000 per individual patient in albeit a rare market that is more one hundred times the size of DGKE patients.
DGKE patients gravitate towards the aHUS community but there is little to be found that is relevant to them other than TMA.
Although globally there may be 70 incidents each year many DGKE patients survive the onset. Over 20 years say, a prevalent patient population of 1500 could accrue many of whom need no treatment. A fraction of which is enough to create a specific patient community within the TMA family but with their own issues and identity and a drive to create their own awareness.
aHUS platforms can help create an embryonic DGKε Syndrome patient movement for a group of people with one genetic problem but two diseases.
Article No. 473