aHUS patient Jaac and his mother Ria are from the UK. Ria spoke to Global Action about her son’s meningococcal infection encounter.
Global Action: Hi Ria when did Jaac become ill with a meningococcal infection?
Ria: It was July last year (2023). Jaac felt very poorly one morning. He was vomiting and began to shake. He was saying he felt cold but was warm to the touch.
So what did you do?
We called a health service helpline for advice and after we explained what he was like they sent an ambulance out to take him to hospital.
My word that escalated quickly. What happened next?
When the ambulance arrived, his temperature had risen again. He was still vomiting and had become very lethargic. Within an hour of first talking to the health service advisers he was in hospital. Once there a rash began to appear. The one that did not disappear when pressed.
Did the doctors know about his aHUS and susceptibility to meningococcal infection?
They told his aHUS consultant and the aHUS Expert Centre in Newcastle upon Tyne about him.
What did the doctors do?
They took blood cultures but those would take 48 hours to get results. We waited and when the results came back, they showed he had a meningococcal infection.
Had he been vaccinated and was he on antibiotics?
Yes, for ACWY and B, he even had meningitis boosters, and that is what the doctors did not understand. He even took penicillin twice a day. The day prior to him becoming ill he had his ravulizumab treatment.
How long had he been treated for aHUS?
By then it had been nearly two years. He was 1 year old when he became ill with aHUS. He had switched from eculizumab to ravulizumab just three months earlier.
So what happened once the infection had been found?
He was taken to a ward and was put on antibiotics for meningococcal disease and spent a week there. By then Jaac had lost his appetite and had become very tired., because of the type of meningococcal infection they had found!
And how is Jaac now?
He is fully recovered now and is bouncing round like a usual 3-year-old boy. He had had to stop all infusions due to this becoming more of a high risk again and goes into hospital weekly for bloods to make sure he does not relapse at any point.
When this all started did you think it might have been a meningococcal infection?
We did not think it was at first as he did not show the usual symptoms, apart from the rash but it was the blood culture test results which confirmed it for us.
But you acted very quickly anyway and that made a difference.
Also the care pathway in this case was exemplary.
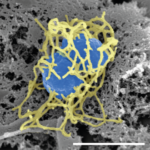
Although fully vaccinated a breakthrough infection is still possible. Whilst not usually infectious, the “ungroupable” types of meningococcal infection i.e. bacteria without encapsulated shells, may on rare occasions cause meningitis or sepsis but an infection responds well to antibiotic treatment.
WARNING: Serious meningococcal infection can happen in patients treated with complement inhibitors. Follow precautions and be vigilant. Keep up to date with vaccines and boosters. Be vigilant and act quickly on possible symptoms
Article No. 633
Previous articles:

Meningococcal Infection – Symptoms
Complement Inhibitor users are the group at most risk of meningococcal infection according to the Centre for Disease Control in the USA. Some of those complement inhibitor users are aHUS…
CONTINUE READINGMeningococcal Infection – Symptoms
aHUS meningococcal infection – vigilance essential
All aHUS patients know that when on complement inhibitor treatment they are at risk of meningococcal infection. Do they? Of course, they are told about it before they get treatment.…
CONTINUE READINGaHUS meningococcal infection – vigilance essential

Some side effect- Meningococcal infection!
The side effects of treatment and residual ailments of an aHUS onset featured highly by aHUS families in the contribution to the aHUS Patients Research Agenda. The topic is covered…

