The Life and works of Prof. Conrad von Gasser continues the series of Before aHUS Endeavours Fade.
Contents
- Introduction
- Early years, education, and training
- Clinical Practice
- Hemolytic Uremic Syndromes
- Later years, death and legacy
- Concluding remarks
- Appendix A – copy of the 1955 Gasser et al article about HUS
- Introduction
This “mini biography” of Professor Johann Conrad Von Gasser builds on a previous article in the Before aHUS Endeavours Fade series on the aHUS alliance Global Action website , www.ahusallianceaction.org.
It has been released to coincide with the 70th anniversary of the first patient to be officially diagnosed using the clinical term haemolytic uraemic syndrome. The seven-month-old patient arrived at the hospital where Conrad practiced in Switzerland in July 1954.
She was severely anaemic and with kidney failure. She died within 30 days of becoming ill, but those three words “hämolytisch-urämische syndrome” in German were typed on her official medical report as Conrad’s diagnosis.
In late 20th and early 21st centuries there were seldom any articles about HUS, and its atypical version, without the name Conrad Gasser appearing in them to define the condition. Why was that? Who was Conrad von Gasser?
1. Early life, education, and training
Johann Conrad Gasser was born on 19 September 1912 in Chur, Switzerland. Chur is a city 80 miles to the southeast of Zurich near the border with Lichtenstein. His parents were Professor George Eduard Gasser (1874 -1953) and Lidia Ribetti (1872-1941). His father was Swiss, and his mother was of Italian descent.1
George Eduard was born in Hallau, a small historic municipal village in the canton of Schaffhausen in Switzerland, about four miles from the border with Germany.2 The Gasser family’s connection with Hallau goes back to the early eighteenth century at least when his five times Great Grandfather Hans Jakob Gasser lived there.3 The name Gasser is still associated with several businesses in Hallau today. Hallau is also still known for its wine making as it was in Hans Jakob’s time.
At some time, Conrad chose to not use the name Johann but would add the term von to the family name. In Germany von can be taken as either as the literal “from” by commoners, or as indicating a noble lineage. As no place called Gasser is associated with Conrad he chose to emphasise his connection to his Gasser lineage. Though none of his immediate ancestors appear to have used the term.
Conrad’s father had a Professorship at the University of Chur where Conrad grew up. He attended schools in Chur until his high school graduation and then he left for Zurich to study medicine. During Conrad’s medical studies he spent time in Rome, Vienna and Berlin. He completed his medical education in 1937 with “habilitation”, the highest university examination in Switzerland. In 1938, after presenting his dissertation “Results of Pneumococcal Infection”, he was awarded his medical doctorate. For the next four years he spent his time training as an assistant in Zurich and St Gallen hospitals, learning about bacteriology, pathological, anatomy and internal medicine.4
In September 1938 he attended an International Conference for Microbioology in New York, USA and was mentioned as a coauthor of a report on the conference published in 1939.5
Chapter 2- Clinical Practice
In 1941 Conrad became a Resident at the Kinderspital Zürich (see image below). It was also known as University of Zurich Children’s Hopital or “KiSpi” as its employees affectionately referred to it. He came under the supervision of Professor Guido Fanconi. Prof. Fanconi, a pioneer of paediatric medicine, was an eminent pediatrician who had become known for describing several haematological disorders in children, including Fanconi Syndrome, a rare kidney disorder.6

Just as Conrad began his new career at the Kinderspital, his mother Lidia was to die suddenly in Rome at the age of 56. It was apparent from her funeral notice that Conrad, who was by then a 29-year-old, had a family, as he and his wife Irene (born Nussberger) and their eldest child Peter attended Lidia’s “silent” funeral along with Conrad’s sisters, Elba (also a doctor) and Wilmer.7
In 1945 Conrad became Chief Resident (Oberartz) in the Kinderspital Medical Department. His workload was heavy and in addition to his clinical and administrative responsibilities he taught and also spent time on haematology research. Conrad would be credited with creating and developing a pediatric haematological department at the hospital. Conrad’s style of clinical examination was described by colleagues as extremely careful and child friendly. He was known by his assistants as someone to pass on to them his personal experience on issues rather than from his knowledge of current literature. It was acknowledged that a lot could be learned from him.6
Soon after becoming Chief Resident, he began to write articles on his two key specialisms, diseases of childhood and haematology. He would write about a diverse range of topics. His early works were usually published in the established Swiss Medical Weekly, or Helevetica Paediatricia Acta which had been newly founded by Prof. Fanconi.6
His first article in 1946 was a case study on the effect of medical interventions for the treatment of chronic myeloid leukaemia in three children.8 Another treatment article followed on the use of a, then very novel, antibiotic called penicillin on children.9 Switching themes his next article was about a collaborative study on the malformation effect of infections and toxins on unborn children.10 He followed that with another different topic of bronchial and viral pneumonia.11 Then he returned to a treatment topic on the use of streptomycin for “Bang’s disease” (Brucellosis),12 before turning to the condition of haemolytic anaemia, which became a topic of great interest to Conrad. He had two articles published on haemolytic anaemia in premature births.13,14
Conrad also contributed a chapter about Foetal Death in a book about Gynecology.15
The scope of his published work continued to widen during the end of the decade to include conditions such as whooping cough,16 meningitis,17, ABO blood type incompatibility18, blood transfusion practice in the new born,19 and a condition that Conrad had discovered, acute erythroblastopenia.20, 21
Throughout the 1940s Conrad’s background research related to haemolysis. In 1949 his book “The Haemolytic Syndromes in Children” was published.22 The book provided a comprehensive overview of a rapidly developing subject. Prof. Fanconi wrote in the book’s introduction, “for almost ten years, his senior physician ( Conrad) had made hemolysis a special interest of research and that Conrad had been the original discoverer of acute erythroblastopenia”. Conrad had carefully documented a wealth of observations of haemolytic anaemia in childhood illnesses. Following the publication of the book, Conrad was awarded a Venia Legendi, i.e. he was given permission to lecture on this subject.4 In time the book was also to be recognised as a significant contribution to the understanding of anaemia in children and to the development of the paediatric haematology specialism in Europe.23
The Venia Legendi provided Conrad with an opportunity to develop an international reputation in the medical world. Later his colleagues were to observe that he had “a wealth of original new ideas”. He had seemed to have inherited a keen sense of logic and ability to get to the bottom of things from his father.4
Publication of Conrad’s varied research interests gathered pace in the early to mid-1950s. Of the 79 published articles that Conrad authored or coauthored, a third were to be published in this part of his career.24 He continued to extend his range of subjects to include articles on thrombocytopenic purpura,25 haemophilia,26 leukaemia,27,28, , various haemolytic anaemia conditions29,30,31.32,, and including a new haemolytic anaemia syndrome identified in fourteen patients33, and two related to new-borns , incompatible blood types diseases34 and as well clinical practices for haemolytic disease35. He even took time to work with his colleague Professor Ettore Rossini to write a tribute to his departmental head, Guido Fanconi, on the latter’s 60th birthday!36
As a teacher Conrad continued to guide the new residents who worked in his large ward “Saal 4”. at the Kinderspital . As part of introducing them to the developing medical discipline of haematology Conrad instructed them to take, measure and study blood samples for themselves.6 One of these residents was Dr Emile Gaultier, who was to come under Conrad’s stewardship in 1952.
At this time Conrad was also in contact and collaborated with the work of Professor William St Clair Symmers of Charing Cross Hospital in London.37 In 1952 Prof. Symmers had described several thrombotic microangiopathic haemolytic anaemias which he shortened to “thrombotic microangiopathy” as a new term.38
Conrad’s haematology services soon developed into a highly respected centre, with patients flocking from all over the world for advice and help. Conrad became intensively involved in the diagnosis and treatment of acute leukaemia, pan myelopathies as well as constitutional and acquired haemolytic anaemias. 6
In April 1953 his father Prof. George Eduard Gasser died at 79 years of age.39
In 1954 Conrad turned his attention to a particular group of children who had experienced haemolytic anaemia but who also appeared to be suffering from kidney failure.
Chapter 3- Haemolytic Uraemic Syndromes
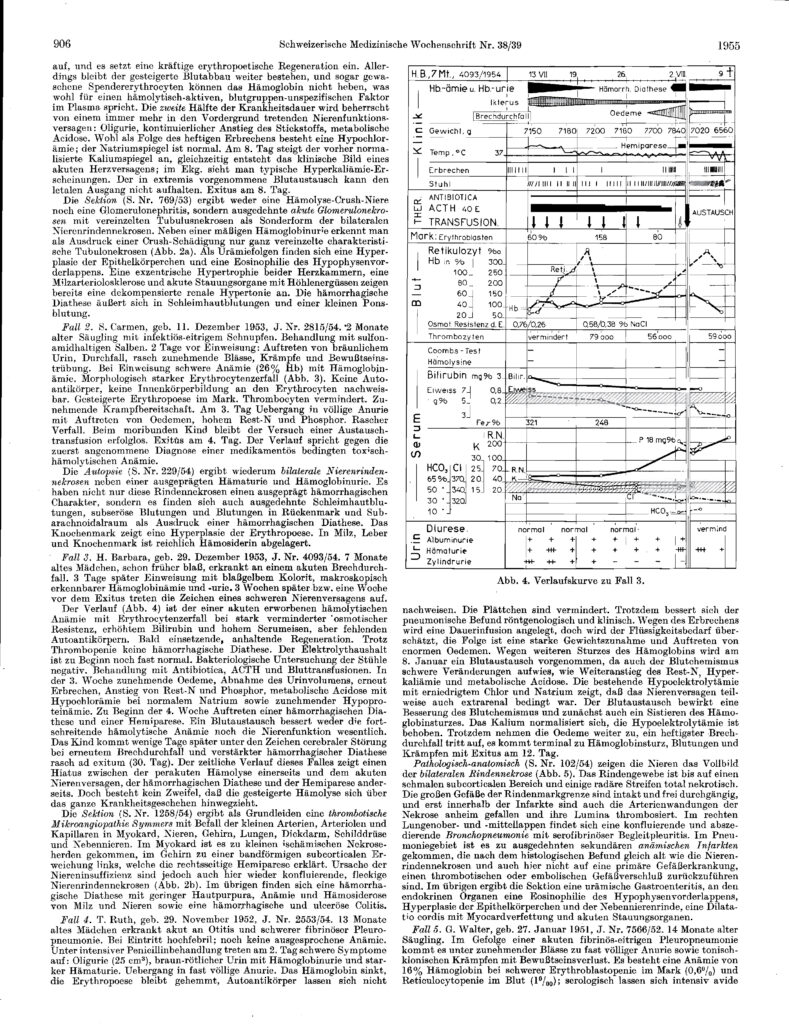
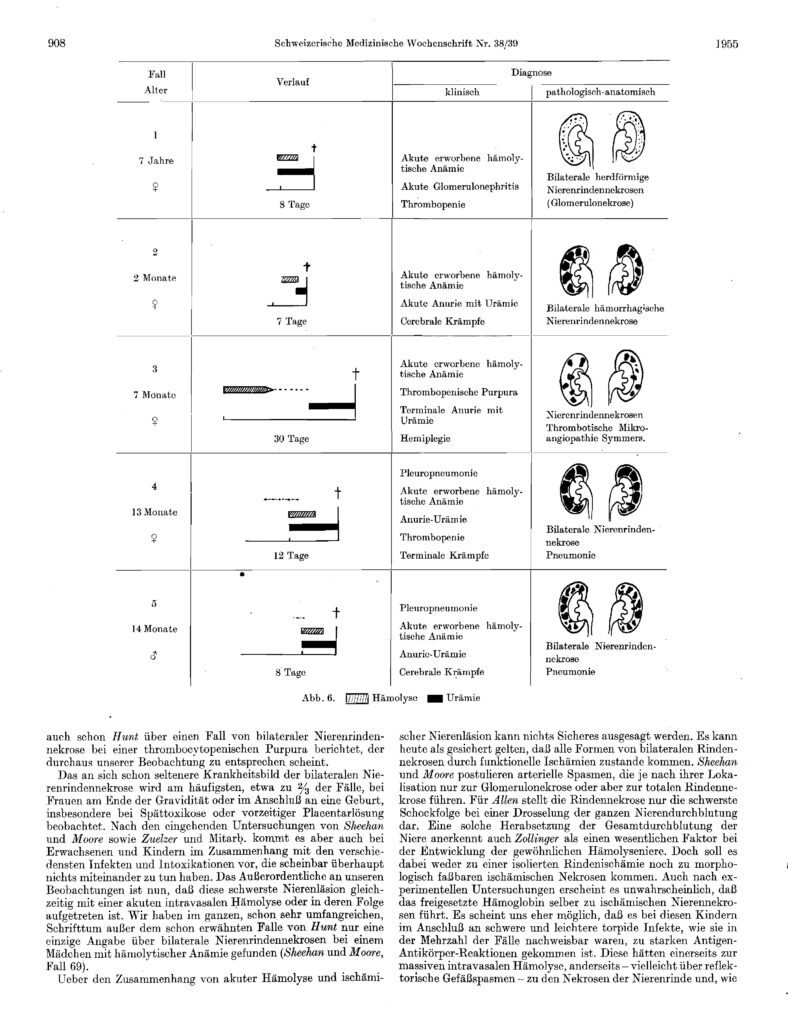
Conrad von Gasser’s seminal work on the description of the Hemolytic Uremic Syndromes was published on 20 September 1955. Written in German and appearing in the Swiss Medical Journal its title was “Hämolytisch-urämische Syndrome- Bilaterale Nierenrindenekrosen bei akut erworbenen hamolytichen Anamien”.40
It was the product of teamwork by Conrad and his Zurich Kinderspital colleagues, Drs Gautier and Steck, and two pathologists , Dr Rudolf Siebenmann and Dr R Oschlin from the Kantonsspital, Zurich. Their work began in early 1954.41
The observations leading up to this research group’s discovery had emerged from the weekly meetings which had been established by Prof. Fanconi along with his residents and the staff of the Pathology Institute in Zurich Kantonsspital. The Kantonsspital had been contracted to provide post-mortem services to the Kinderspital. Dr Siebenmann was employed by the Pathology Institute in January 1954 and was given responsibility for the postmortem services to Kinderspital and to attend meetings in which the results were discussed. As both clinical and laboratory aspects were studied at these meetings they were described as “clinicopathological confrontations”. Rudolf Silbermann recalled that they were attended by Conrad, and Doctors Ettore Rossi and Andrea Prader. He remarked how he looked back fondly on the work of this group because he found that the paediatricians were so interested in his autopsy findings.
In 1954 five young patients, who had died at the Kinderspital, became of specific interest to Conrad and his colleagues. In Figure 2, the headings of the front page of the health records of four of these children are shown in the image below. Their diagnosis is described. The handwriting on these records is that of Conrad and had been added after the post-mortems had been carried out.
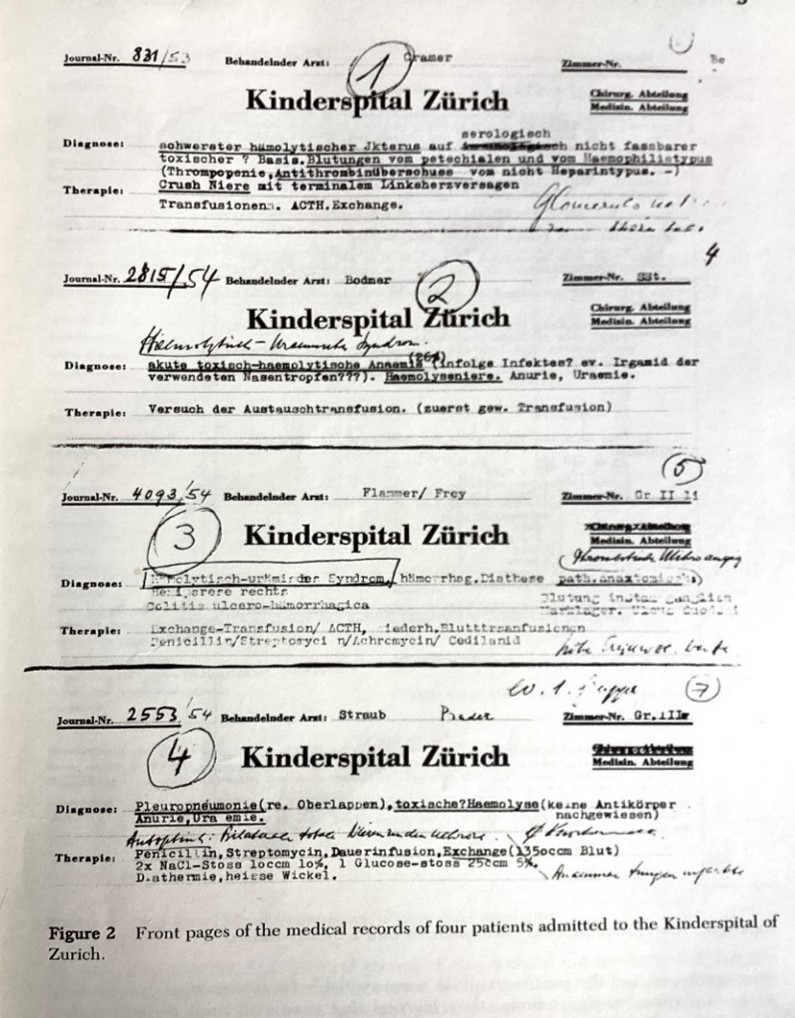
Record 3 (4093/54) is of a child called Flammer/Frey whose first name was Barbara , and who was just 7 months of age and had been admitted in July 1954. She died within 30 days of first becoming ill. In her medical record her diagnosis has been typed and the term haemolytic uraemic syndrome is used officially for the first time as the cause of illness. The disease name was typed in German “hämolytisch-urämische Syndrom” and had been created by Conrad for this fatal case. Dr Oschlin performed the autopsy.
Record 2 Journal No. 2815/54 is of a patient, a girl named Bodmer, admitted as an emergency to the hospital in February 1954 but later her original diagnosis has been corrected in writing by Conrad. It is not known when.
One of Dr Siebenmann’s first autopsies on his arrival at the Institute earlier that year was of a 13-month-old child who was found to have bronchopneumonia and who had died 12 days after admission to the hospital. Siebenmann found the child had anaemia and kidney failure. The autopsy had revealed an unusual “infarct ischenmia in the lungs and thrombi in the glomeruli”. Thrombi were only found in the arteries and veins of the kidney and the area of the lung infarction. Record 4 2553/ 54 is of this child, whose family name was Pradet, and who was added to the group of interest to the research team .
By July 1954 the term “Hemolytic Uremic Syndromes” had been created and other potential cases of children with the illness were being identified. Conrad asked Dr Siebenmann to review the pathology of Records 2 and 3 and six other infants who had died of what he thought was the same clinical entity. In three of the other six cases Dr Siebenmann found similarities with the children Flammer/Frey and Bodmer, including the child Pradet in Record 4 and two others. One of the two patients became Record 1 831/53 of a child name Cramer who had been admitted to the hospital in 1953. Another record of a fifth child included in the study, who had been admitted earlier in 1952, has subsequently been lost but Siebenmann had found comparative evidence of HUS in that child too.
The research group had gathered evidence from the five records that there was a common theme of mechanical anaemia, low platelets and kidney failure in the cause of death in these children. Thanks to Conrad they now had a term to describe their illnesses i.e. Haemolytic Uraemic Syndromes.
On a cold winter evening in late 1954 Siebenmann and a colleague visited the Kinderspital and met in Conrad’s office with Conrad and two of his colleagues, Doctors Gaultier and Steck. That night they decided to write a paper about what they had found.
Conrad and Siebenmann presented a joint paper at the 10th Annual Meeting of the Swiss Society of Haematology in Geneva in May 1955. Gasser describing the clinical findings and Siebenmann the pathological discoveries.40 A shortened version of their presentation was subsequently published in the Schweizerische Medizinische on 20 September later that year. 39
Looking back and with knowledge of subsequent work done by others Siebenmann has acknowledged that the syndromes were not necessarily fatal. Kidney cortical necrosis was not always found and that the small thrombotic microangiopathy was more frequent and it was the cause of any kidney cortical necrosis. Siebenmann admitted that one of the cases was probably a pediatric case of TTP. He defended the fatality claim by saying that the detection and description of a new syndrome is often based on observations in the more severe form of a disease. He claimed that the collaboration with Conrad was a good example of clinicopathological cooperation and it was of importance to general pathology too.41
Unlike Fanconi and others including Doctors Hans-Ulrich Zellweger , Manes Kartagener, Eugene Boltshauser , Andrea Prader and Heinrich Willi, who had been Residents at the Kinderspital, Conrad was not to give his name to the disease he had been the first to describe.42 There would be no Gasser Syndrome
.Chapter 4 Later years, death and legacy
In early 1955 Conrad delivered a slide presentation about poliomyelitis at a meeting in Zurich to encourage take up of vaccinations against the disease. He covered the serious side effects of the disease including the paralysis it caused in the lungs necessitating the use of the so called “iron lung” ,of which, he emphasised, there were only six devices in all of Switzerland. 43
Conrad was awarded the Finlay Medal for blood research in October 1955. The Finaly Medal, awarded annually , is named after the discoverer of the yellow fever pathogen. 44
In 1956 Conrad after eleven years as senior physician left the Kinderspital. At that point in his career, he could have expected to have reached medical director elsewhere, but it was not to be. Professor Fanconi did not retire until 1965.6 So Conrad set up a private medical practice a short distance away from the hospital at 121 Freiestrasse, Zurich. In June 1956, he advertises himself as a specialist for children disease and citing his experience as a haematology consultant at the hospital and university in Zurich.45
His research publications tapered off following his move into private practice. In the remainder of the 1950s he wrote about childhood leukaemia treatment46, vaccinations in childhood47 and Heinz body anaemia.48
He gave talks on Swiss Radio, talking about ABO blood type incompatabilities.49
In June 1962 he began teaching at the University of Zurich as he had become an adjunct Professor of Paediatrics. Students, assistants, and nurses, as well as physicians (in the advanced training courses) benefited greatly from his extensive knowledge.50
He remained Treasurer of the European Society of Hematology until 1968 when after 13 years in the role he stepped down. In his capacity as Treasurer Conrad organised and chaired three symposia on paediatric haematology.4
By the1960s his published work became less frequent but included more topics including meningosis52, auto immune haemolytic anaemia53 and lymphocytes in children.54 He also reprised his HUS work which was included in a handbook 55 ,and a book 56 remaining keen to point out the differences between his syndrome and TTP.
In November 1971, in recognition of his scientific attainment, he was appointed to the Scientific Advisory Board of the German Society of Hematology.57 Election to President of the Society of Hematology was to follow.4 His international reputation continued to grow.
His wife Irene died at 56 years of age in February 1973. She had been a journalist for a local newspaper. Conrad attended the funeral with his children Peter, Conrad, Anne-Marie, Christine and grandchildren.58
Conrad ended his civic role on the Zurich Canton Council in December 1977. He was Senior Physician at the Institute of Anaesthesiology at the Zürich Cantonal Hospital at the time.59
In 1977 Conrad had written to Professor Bernard Kaplan, and his colleague Professor Keith Drummond, requesting copies of their papers on HUS 60 [this was before the days of the Internet]. Prof. Kaplan sent him reprints and invited Conrad to visit the Montreal Children’s Hospital. 61
Throughout the 1970s Conrad’s written work became less frequent. Two of his articles were about panmyelophies 62.63 and a third was about another new syndrome he had found, conatal insufficient erythropoiesis with circumscribed anomalies. 64
Conrad was to visit Montreal in 1978 , see image below with Conrad at centre, Prof. Kaplan recalled him giving a memorable lecture on his syndrome. He said that ”Conrad , a pediatric hematologist, was a gracious, thoughtful and generous man”. He told us about his interest in the anaemias and how he had noticed that some children with acute anaemia had bizarre, shaped erythrocytes. These fragmented red blood cells were called schistocytes. He and his co -workers, to whom he gave unstinting credit, selected five cases, which, in addition to evidence of hemolysis were severely ill with thrombocytopenia, acute renal failure and cerebral symptoms. All five patients died. Four had vomiting and diarrhoea and one had pneumonia. Gasser believed and continued to stress in his lecture as well as in a chapter in 1978, that the essential feature that distinguished HUS from Thrombotic Thrombocytopenia [TTP] was the severe renal involvement in the former, and the multi-organ involvement in the latter. 65
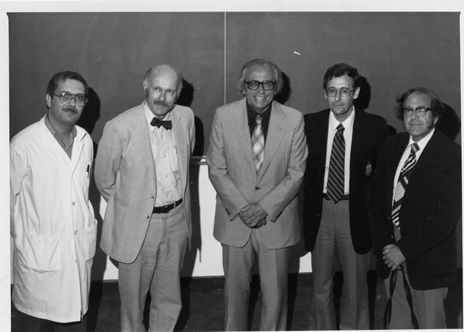
At their meeting in 1978 Conrad congratulated Keith Drummond (Bernard ‘s Montreal mentor] and Bernard for their editorial titled “The hemolytic-uremic syndrome is a syndrome”.60 However, he gently chided them because he pointed out that his original paper was not entitled Haemolytic Uraemic Syndrome but Haemolytic Uraemic Syndromes. In German, he explained, Syndrom is the plural for syndrome. However, Conrad was generous in his praise for the fact that they had restated his concept. Conrad presented Bernard with a Swiss cowbell, see image below,and asked him to ring it whenever the first International Symposium on HUS was to be held.4

In October 1980 Conrad was appointed as a Fellow of the International College of Paediatrics.66 In the same year he published what was to be his final article. Again, it was about the long-term survival of 11 children who had survived acute leukaemia and whom he had monitored for up to 28 years “9 as outpatients to avoid the danger of hospital infections and to give them a better psychological ambiance. 3 grown-up patients had become parents themselves of altogether 6 children, which proves the possibility of normal progeny.” 67
In the latter years of his career Conrad was invited increasingly to give guest lectures at national and international congresses and to participate in round table discussions. His enormous experience in the treatment of acute leukaemia made it possible to achieve the longest survival times; this earned him special respect.4
On the 2nd of August 1982, just before his seventieth birthday, and after a dignified endurance of a long illness, Conrad died.68
He was buried on the 6th of August at the Reformation Church in Husnacht a town just south of Zurich. His funeral was attended by his sister Elba and his children Peter, Conrad , Anne-Marie and Christine. Also, his grandchildren Fabian, Christopher and Sabine. His friends and colleagues attended in large numbers too. Pastor Mockli conducted the service and ably captured the life mission of Conrad, about whom Professor. K Betke from Munich also spoke movingly.69
His old colleague from the Childrens’ Hospital Ettore Rossi presented Conrad’s obituary which was published in the local newspaper. He wrote that “Swiss paediatrics had lost one of the most important personalities with an extraordinary international reputation”. He also said that his friends and colleagues “mourned an irreplaceable loss with Conrad’s passing and that they could cherish the most beautiful memories of someone who had brought a lot to the job”.4
In September 1982 Bernard Kaplan sent a letter to Conrad to inform him of his intention to dedicate the first symposium on HUS at an international conference to him. He had not known of Conrad’s death a month before his letter reached Conrad’s office. 61 And so, in Hannover, Germany in 1983 Bernard rang Conrad’s cowbell in his honour and memory. 70
In 1995 Conrad was to be published again for a final time when posthumously the 1955 article was to be included in a 125th anniversary edition of Swiss Medical Weekly. 69
Years later on 9th September 2015 Bernard Kaplan presented a Grand Rounds lecture at The Hospital for Sick Children, Toronto. Its title was “Re-imagining the Hemolytic Uremic Syndrome” and he talked again about the cowbell that Conrad had given him.70
Bernard said that Conrad and his colleagues had differentiated HUS from TTP [although it took about 50 years for this to become accepted fully] and described what it is now recognised as Streptococcal Pneumoniae HUS, and “familial” HUS, recurrent HUS or aHUS. Although many of their patients had diarrhoea and vomiting Conrad did not recognise the diarrhoea as a prodromal feature of HUS.65 Nor at that time, was Conrad aware of Shiga Toxin E.Coli as being a trigger of the HUS in his cases. Though eventually STEC HUS would become synonymous with HUS and the term atypical HUS would be used for everything else.
6. Concluding remarks
Johann Conrad von Gasser was privileged to be born into medically educated family and began a career in an era when his country was not directly involved in a global conflict. His career was starting at a time when he could be a part of the rapidly developing clinical movement in paediatric haematology. He had an eminent leader in the subject as a mentor but with a personal drive for specific research to understand more about hemolysis.
Determined to use his personal intellectual skills of analysis and drilling down to get to the nub of an issue. He was surrounded by colleagues who were major players in early European pediatric haematology research.
Although Conrad’s work on a particular hemolysis associated with kidney disease was possibly to be his best known, its discovery within the context of his wider research work on leukaemia, haemolytic anaemia and erythroblastopenia was probably not something that would be of particular extra significance to him at the time . It was for others to recognise that in years to come. Although he led no further on the matter he continued to watch and follow what others were doing but did not add to his original discovery.
A manifestation of the “triad” of haemolytic anaemia, thrombocytopenia and kidney injury might suggest a possibility of a haemolytic uraemic syndrome diagnosis is now established in current diagnosis protocols. Also, after 70 years it has become the root in the name of a larger number of HUS conditions. Proving Conrad right to be cautious about his nomenclature by using the plural of the term for baby Barbara Flammer/Frey’s diagnosis in that summer of 1954.
APPENDIX A- A copy of the 1955 article by Gasser et al about HUS



References
- Conrad Gasser – Wikipedia, the free encyclopedia (2023) (accessed 8 May 2024)
- Hallau – Wikipedia (2024) ( accessed 8 May 2024)
- Public Family Trees – Ancestry.com (accessed 8 May 2024)
- Rossi E., Zum Tode von Conrad Gasser On the death of Conrad von Gasser , Neue Zürcher Zeitung, 5 August 1982, page 31, http://www.e-newspaperarchives.ch/?a=d&d=NZZ19820805-01.2.38.9 (Accessed 8 May 202
- Gasser C., and others International Congress for Microbiology , Schweizerische Zeitschrift für allgemeine Pathologie und Bakteriologie (1938) 1 (1-6): 94. https://doi.org/10.1159/000158273
- Hitzig W., H., Chronik der hamtologisch-immunologischen Abteilung des Universitats-Kinderspitals Zurich 1945-1989, (2015), Neujahrsblatt_NGZH_2015.pdf
- Death of Lidia Gasser-Ribetti Neue Zürcher Zeitung 15th October 1941 page 7 http://www.e-newspaperarchives.ch/?a=d&d=NZZ19411015-03.2.25.2 ( Accessed 8 May 2024)
- Gasser C., Three cases of chronic myeloid childhood leukemia with special attention to the effects of X-Rays and splenectomy on blood count and bone marrow. Helvetica Paediatrica acta , May 1946
- Gasser C., Penicillin in der Kinderheilkunde [Penicillin in pediatrics]. Ann Paediatr. 1946 Nov;167(5):273. German. PMID: 20340319.
- Gasser C, Schwarz E. Foetale Missbildungen mit abnormen Verkalkungen als Folge intrauteriner Infektionen (Toxoplasmose, Röteln in graviditate usw.) [Fetal malformations with abnormal calcifications as a result of intrauterine infections (toxoplasmosis, rubella in graviditate, etc.)]. Helv Paediatr Acta. 1947 Aug;2(4):351-70. German. PMID: 20260461
- Gasser C. Die Wassermann-positive Bronchopneumonie im Kindesalter und ihre besonderen Verlaufsformen (Syndrom Fanconi-Hegglin) Beitrag zur Kenntnis der miliaren Bronchopneumonie und Virus-pneumonie [Aquarian-positive bronchopneumonia in childhood and its special forms (Fanconi-Hegglin syndrome) contribute to the knowledge of the bronchial pneumonia and viral pneumonia]. Helv Paediatr Acta. 1947 Jun;2(3):185-226. German. PMID: 20260449.
- Gasser C. Erfolgreiche Streptomycintherapie bei einem Fall von Morbus Bang [Successful streptomycin therapy in a case of Bang’s disease]. Ann Paediatr. 1948 Nov-Dec;171(5-6):400. German. PMID: 18105623
- Gasser C, Karrer J. Deletäre hämolytische Anämie mit Spontan-Innenkörper-Bindung bei Frühgeburt [Delicate hemolytic anemia with spontaneous inner-body binding at premature birth]. Helv Paediatr Acta. 1948 Nov;3(5):387-403. German. PMID: 18101056.
- Gasser C. Spontaninnenkörperbildung mit deletärer hämolytischer Anämie bei Frühgeburt [Spontaneous internal body formation with deleterious hemolytic anemia in premature birth]. Ann Paediatr. 1948 Nov-Dec;171(5-6):392. German. PMID: 18105621.
- Gasser C. Zum Thema, Intrauteriner Fruchttod [To the Subject of . . . Intrauterine fetal death]. Gynaecologia. 1949 Dec;128(6):371-85. German. PMID: 15409112.
- Willi H., Gasser C., Observations on 64 cases of whooping cough treated with chloramphenicol , Annales Paeditrici May 1951, International review of paediatrics
- Gasser C., ROSSI E., and PICHLER H. Die Therapie der eitrigen Meningitiden im Kindesalter [Therapy of purulent meningitis in childhood]. Helv Paediatr Acta. 1947 Nov;2(5):405-42. German. PMID: 20273235
- Grumbach A, Gasser C. ABO-Inkompatibilitäten und Morbus haemolyticus neonatorum [ABO incompatibilities and haemolyticus neonatorum]. Helv Paediatr Acta. 1948 Dec;3(6):447-74. German. PMID: 18107031
- Gasser C. Zur Technik der Exchange-Transfusion beim Neugeborenen [The technology of exchange transfusion in the newborn]. Helv Paediatr Acta. 1949 May;4(2):182-4. German. PMID: 18151688
- Gasser C. Akute Erythroblastopenie; 10 Fälle aplastischer Erythroblastenkrisen mit Risenproerythroblasten bei allergisch-toxischen Zustandsbildern [Acute erythroblastopenia; 10 cases of aplastic erythroblast crises with Risenproerythroblasten in allergic-toxic condition pictures]. Helv Paediatr Acta. 1949 May;4(2):107-43. German. PMID: 18151683.l
- Gasser. Akute Erythroblastopenie [Acute erythroblastopenia]. Schweiz Med Wochenschr. 1949 Sep 10;79(36):838-40. German. PMID: 18140912
- Gasser C., Haemolytic Syndrome in Children ( 1949), G Thieme, Stuttgart, Die hamolytischen Syndrome im Kindesalter; : Gasser, Conrad Johann, 1912- : Free Download, Borrow, and Streaming : Internet Archive (accessed 8 May 2024_
- Pearson, H. History of Pediatric Hematology Oncology. Pediatr Res 52, 979–992 (2002). https://doi.org/10.1203/00006450-200212000-00026
- Database of Conrad Gasser Articles – C. Gasser | Semantic Scholar (accessed 12 June 2024)
- Gasser C, Hollander L. Akute, durch Autoantikörper bedingte hämolytische Anämie, einhergehend mit thrombocytopenischer Purpura bei einem Säugling [Acute hemolytic anemia associated with thrombocytopenic purpura caused by autoantibodies]. Ann Paediatr. 1952 May-Jun;178(5-6):340-2. Undetermined Language. PMID: 14953021.
- Cramer, R., Fluckiger, P., Gasser, C., Koller, F., Loeliger, A.E., & Matter, M. (1953). [Hemophilia B; two cases of hereditary hemophilia due to a deficiency of a new clotting factor (Christmas factor)]. Acta haematologica, 10 2, 64-76 .
- Gasser C. Behandlung der Leukämie im Kindesalter mit Cortison und Aminopterin [Therapy of leukemia in children with cortisone and aminopterin]. Schweiz Med Wochenschr. 1953 Oct 3;83(40):957-9. Undetermined Language. PMID: 13101677.
- Gasser C, Cramer R (1953) Leukämie im Kindesalter unter Cortison und Aminopterin. Helv Paed Acta 8:10—89
- Gasser C. Beziehungen zwischen erworbener hämolytischer Anämie und aplastischer Anämie [The relationship between acquired hemolytic anemia and aplastic anemia]. Bibl Paediatr. 1954;58:630-5. German. PMID: 13229973
- Bonham-Carter RE, Cathie IA, Gasser C. Aplastische Anämie (chronische Erythroblastophthise) bedingt durch Autoimmunisierung [Aplastic anemia (chronic erythroblastophthisis) caused by autoimmunization]. Schweiz Med Wochenschr. 1954 Sep 25;84(39):1114-6. German. PMID: 13216156
- Gasser C. Pure red cell anemia due to auto antibodies; immune-type of aplastic anemia, erythroblastopenia. Sang. 1955;26(1):6-13. PMID: 14358527.
- GasserC. Erythroblastopénie aiguë dans les anémies hémolytiques [Acute erythroblastopenia in hemolytic anemia]. Sang. 1950;21(3):237-45. Undetermined Language. PMID: 15418101
- Gasser C. Die hämolytische Frühgeburtenanämie mit spontaner Innènkörperbildung; ein neues Syndrom, beobachtet an 14 Fällen [The hemolytic anemia of premature infants with spontaneous Heinz body formation; a new syndrome observed in 14 cases]. Helv Paediatr Acta. 1953 Dec;8(6):491-529. Undetermined Language. PMID: 13151592
- Gasser C. Maladie hémolytique du nouveau-né due aux groupes ABO [Hemolytic disease of the newborn due to ABO groups]. Rev Hematol. 1955;10(2):253-4; discussion, 256-64. French. PMID: 13255422.
- Gasser C. Das Vorgehen bei Morbus haemolyticus neonatorum (Rh) in der Praxis und im Spital [The procedure in hemolytic disease of the newborn in practice and in the hospital]. Praxis. 1955 Jul 14;44(28):640-6. German. PMID: 13245617
- Gasser C, Rossi E. Herrn Prof. Dr. Guido Fanconi zum 60. Geburtstag am 1. Januar 1952 [On the 60th birthday of Prof. Guido Janconi, on the 1st January 1952]. Schweiz Med Wochenschr. 1951 Dec 2 9;81(52):1289-90. Undetermined Language. PMID: 14913096
- Sparta, G. Haemolytic Uremic Syndrome: From Bedside to Bench to Bedside, Posted at the Zurich Open Repository and Archive, University of Zurich, July 2018, Habilschrift_Sparta_Nephrologie_Zora_220120.pdf (uzh.ch) (Accessed 20 June 2024)
- Symmers WS. Thrombotic microangiopathic haemolytic anaemia (thrombotic microangiopathy). Br Med J. 1952 Oct 25;2(4790):897-903. doi: 10.1136/bmj.2.4790.897. PMID: 12978378; PMCID: PMC2021829
- Death Notice Prof.Dr.phil George Edward Gasser Neue Zürcher Zeitung, No.1000, 30 April 1953, page 10 Untitled — Neue Zürcher Zeitung 30 April 1953 Edition 03 — e-newspaperarchives.ch (accessed 12 June 2024)
- (a)Gasser, C., Gautier, E., Steck.A., Siebenmann, R.E., and Oechslin, R. Hamolytisch-uramische Syndrome: Bilateral Nierenrindenneckrosen bei akuten erworbenen hamolytischen Anamien. Schweiz, Med Wochenschr, 85, 905 (1955
- Gautier E, Siebenmann RE. The Birth of the hemolytic uremic syndrome. In. Hemolytic uremic syndrome and thrombocytopenic purpura. Eds Kaplan BS, Trompeter RS, Moake JL. Marcel Dekker, Inc. New York, 1992
- Huisman LM, Huisman TAGM. World-Renowned “Swiss” Paediatricians, Their Syndromes, and Matching Imaging Findings: A Historical Perspective. Children (Basel). 2023 Oct 9;10(10):1668. doi: 10.3390/children10101668. PMID: 37892331; PMCID: PMC10605885
- Gasser C., Public Lecture, Poliomyelitis, Die Tat , 11 February 1955, Page 4, Die Tat 11 February 1955 — e-newspaperarchives.ch (Accessed 20 June 2024)
- Honours, Der Bund, Vol. 106, No.477, 12 October 1955, Edition 2, Page 2. Ehrung von Aerzlen — Der Bund 12 October 1955 Edition 02 — e-newspaperarchives.ch
- Advertisement Dr.med.Conrad Gasser, Die Tat , 9 June 1956, page 9 Die Tat 9 June 1956 — e-newspaperarchives.ch ( accessed 12 June 2024)
- Gasser C, Velasco JA. Las leucemias infantiles y su tratamiento actual [Childhood leukemia and the current treatment]. Rev Esp Pediatr. 1956 May-Jun;12(3):383-99. Spanish. PMID: 13379884
- Gasser C. Impfungen im Kindesalter [Vaccinations in childhood]. Praxis. 1956 Jul 12;45(28):630-8. German. PMID: 13349991.
- Gasser C. Heinz body anemia and related phenomena. J Pediatr. 1959 May;54(5):673-90. doi: 10.1016/s0022-3476(59)80131-1. PMID: 13642237.
- Radio Lecture about blood incompatibility on Studio Zurich, Neue Zürcher Zeitung, 25 January 1957 , No. 215, page 14 Radio — Neue Zürcher Zeitung 25 January 1957 — e-newspaperarchives.ch ( accessed 12 June 2024)
- Government Council — Neue Zürcher Nachrichten 16 June 1962 Edition 03 — e-newspaperarchives.ch ( aAccessed 27 June 2024
- 51.GASSER C. [Meningosis leucaemica]. Schweiz Med Wochenschr. 1960 Oct 22;90:1193-7. German. PMID: 13703851
52. GASSER C. [Autoimmune-hemolytic anemia and related diseases]. Arch Ital Pediatr Pueric. 1960;20:403-6. German. PMID: 13703850.
53.GASSER C. [Lymphocytes in children. Clinico-hematological considerations]. Schweiz Med Wochenschr. 1961 Oct 7;91:1169-81. German. PMID: 13897192
54. Gasser C (1967) Hämolytisch-urämisches Syndrom. In: Opitz H, Schmid F (eds) Handbuch der Kinderheilkunde. Springer, Berlin, Heidelberg, New York, pp 951—963
55. Gasser C. Das hämolytisch-urämische Syndrom [The hemolytic-uremic syndrome]. Ther Umsch. 1968 Aug;25(8):433-7. German. PMID: 5729307
56. Professional Appointment, Neue Zürcher Zeitung, 23 November 1971, Vol 67 No. 274, page 5, Neue Zürcher Nachrichten 23 November 1971 — e-newspaperarchives.ch ( accessed 12 June 2024)
57.Death Notice of Isabel Gasser- Nussberger, Neue Zürcher Zeitung , No.77, page 32, 16 February 1973 Untitled — Neue Zürcher Zeitung 16 February 1973 — e-newspaperarchives.ch (accessed 8 May 2024)
58.Civic announcement, Neue Zürcher Zeitung , No.274, page 48, 22 November 1977, Government Council — Neue Zürcher Zeitung 22 November 1977 — e-newspaperarchives.ch (acced 8 May 2024)
59. Kaplan, B.S. et al. (1984). Haemolytic Uraemic Syndromes. In: Brodehl, J., Ehrich, J.H.H. (eds) Paediatric Nephrology. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-69863-7_20
60. Kaplan, B., S., Drummond, K., N., The Hemolytic-Uremic Syndrome Is a Syndrome, April 27, 1978,N Engl J Med 1978;298:964-966 DOI: 10.1056/NEJM197804272981710, VOL. 298 NO. 17
61. Gasser C. Besonderheiten der kindlichen Panmyelopathien [Special features of childhood panmyelopathies]. Schweiz Med Wochenschr. 1970 Nov 14;100(46):1948-51. German. PMID: 5507833..
62. Gasser C. Erythroaplasie und panmyelopathie im kindesalter [Erythroaplasia and panmyelopathy in childhood]. Hamatol Bluttransfus. 1975;16:193-215. German. PMID: 1193441
63. Hansen HG, Gasser C. Uber ein Syndrom konnatal insuffizienter Erythropoese mit umschriebenen Fehlbildungen [A syndrome of connatal insufficient erythropoiesis with circumscribed anomalies]. Monatsschr Kinderheilkd (1902). 1978 May;126(5):279-81. German. PMID: 651913.
64. Kaplan B.S et al Introduction to Hemolytic uremic syndrome and thrombocytopenic purpura. Eds Kaplan BS, Trompeter RS, Moake JL. Marcel Dekker, Inc. New York, 1992
65. Academic Honours, Neue Zürcher Zeitung, No. 233, 7 October 1980, page 46 , Neue Zürcher Zeitung 7 October 1980 — e-newspaperarchives.ch (Accessed 12 June 2024)6
66. Gasser, C. (1980). Long-term survival (cures) in childhood acute leukemia. Follow-up of nine cases of acute lymphatic leukemia and two of acute myelogenous leukemia with complete remission lasting more than 10 years, three of them with normal progeny. Paediatrician, 9 5-6, 344-57 .
67. Notice of Death and Funeral , Neue Zürcher Zeitung, No 178, 4 August 1982, page 32, Untitled — Neue Zürcher Zeitung 4 August 1982 — e-newspaperarchives.ch
68. Heartfelt Thanks, Neue Zürcher Zeitung, No 189 Page 38, Untitled — Neue Zürcher Zeitung 17 August 1982 — e-newspaperarchives.ch (Retrieved 12 June 20240
69. Gasser C, Gautier E, Steck A, Siebenmann RE, Oechslin R. Wissenschaftliche Rosinen aus 125 Jahren SMW. Hämolytisch-urämische Syndrome: bilaterale Nierenrindennekrosen bei akuten erworbenen hämolytischen Anämien. 1925 [Scientific raisins from 125 years SMW (Swiss Medical Weekly). Hemolytic-uremic syndrome: bilateral kidney cortex necrosis in acute acquired hemolytic anemia. 1925]. Schweiz Med Wochenschr. 1995 Dec 26;125(51-52):2528-32. German. PMID: 8571107.
70. Kaplan, B.S. et al. (1984). Haemolytic Uraemic Syndromes. In: Brodehl, J., Ehrich, J.H.H. (eds) Paediatric Nephrology. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-69863-7_20
Article No.

