In making a choice aHUS patients’ preferences among treatments like eculizumab (and its biosimulars) , ravulizumab, crovalimab, and iptacopan it largely depend on factors such as dosing frequency, effectiveness, safety profile, administration method, and potential side effects.
Starting with eculizumab here’a breakdown of what might influence their preferences for each option:
Eculizumab (Soliris) or approved biosimulars:
• Administration: IV infusion every two weeks with a health care practitioner.
• Patient Preference Factors: Eculizumab was the first approved complement inhibitor for aHUS and has been widely used with established efficacy in preventing thrombotic microangiopathy (TMA) in aHUS patients. It has helped a lot of patients over the past decade or more. However, frequent IV infusions (biweekly) are often burdensome for patients, particularly for those who require regular hospital visits.
• Pros: Proven efficacy and long-term safety data.
• Cons: Frequent dosing schedule; increased infection risk, especially meningococcal infections.
Next up Ravulizumab (Ultomiris):
• Administration: IV infusion every 8 weeks (after initial loading dose). Again with a health care professional assistance.
• Patient Preference Factors: Ravulizumab is a next-generation version of eculizumab with a much longer half-life, allowing for less frequent dosing. Many patients prefer ravulizumab over eculizumab because of its once-every-eight-week schedule, which reduces the need for hospital visits and potentially improves quality of life.
• Pros: Comparable efficacy to eculizumab with a more convenient dosing schedule; reduces healthcare burden.
• Cons: Similar infection risk profile as eculizumab.
Soon will be the availability of Crovalimab:
• Administration: Subcutaneous injection, potentially once every four weeks.
• Patient Preference Factors: Crovalimab, still under investigation, has the advantage of subcutaneous (under-the-skin) administration, which could enable patients to manage their treatment at home themselves.This approach would be particularly appealing to those who wish to avoid frequent IV infusions and hospital visits and spend less time doing it when it is most convenient.
• Pros: Potential for at-home administration with fewer frequent doses; easier to use.
• Cons: Not yet as widely available or as established in clinical practice as eculizumab and ravulizumab.
Also Iptacopan is on its way.
• Administration: Oral tablet, taken daily.
• Patient Preference Factors: Iptacopan is an oral small-molecule drug and represents a new therapeutic approach targeting a different part of the complement pathway (factor B). An oral option like iptacopan could be a major advantage for patients who prefer the convenience of a daily pill over infusions or injections, giving it potential for preference among patients.
• Pros: Convenience of oral administration; new mechanism that could be promising in efficacy.
• Cons: Limited long-term data; potential unknowns regarding safety and effectiveness compared to more established treatments. Does blocking more functions of complement which are still continue with just C5 blocking have more of an impact on patients
All in all patients choice depends on what matters most to them including the:
•Convenience and Reduced Hospital Burden: Patients often favour treatments that minimize the need for hospital visits. Ravulizumab is often preferred over eculizumab due to the extended interval between infusions. Crovalimab, with subcutaneous administration, and iptacopan, with oral dosing, are also likely appealing.
• Safety and Side Effect Profiles: For patients with a high concern for infection risks, or side effects, any treatment that offers similar efficacy with a less other impacts would be preferred.
• Long-Term Efficacy and Trust in Data: Eculizumab remains a trusted option due to its established efficacy and longer history of use, which some patients may prioritise despite the frequency of dosing. This might also apply to biosimulars of eculizumab.
In essence as long as they work as well for treating their aHUS patients generally prefer treatments that offer a balance between efficacy, lower dosing frequency, reduced need for medical supervision, and convenience. As more data emerges, especially for crovalimab and iptacopan, preferences may shift depending on how these newer options align with patient lifestyle and treatment goals.
So far some aHUS patients have had the opportunity to choose or switch between treatments, particularly as new options like ravulizumab and crovalimab become available in more regions. These choices are often influenced by individual circumstances, such as access to healthcare, insurance coverage, clinical trial availability, and, crucially, personal preference for convenience and quality of life.
Moving from eculizumab to eculizumab after ravulizumab received approval as a longer-acting alternative to eculizumab, patients on eculizumab were often offered the chance to switch. Many have preferred ravulizumab due to its extended 8-week dosing interval, which reduces the need for hospital visits and infusion appointments. This is what early transition patients said at the time in research carried out by Global Action.
Similar studies and real-world patient surveys have shown that a significant number of aHUS patients who switch to ravulizumab report higher satisfaction due to the decreased frequency of infusions and overall convenience.
Some patients have been able to access crovalimab and iptacopan through clinical trials or compassionate use programs. The ability to administer crovalimab subcutaneously at home (and potentially iptacopan orally) is a compelling factor for many patients who prioritize independence from hospital-based care. Having a “ locus of control of treatment can have significant positive impact on a patient’s self esteem. Crovalimab trials have drawn particular interest from patients seeking alternatives that align better with at-home treatment and fewer interruptions to daily life.
For younger aHUS patients, the frequency and setting of treatment administration (in-hospital vs. at home) can be particularly impactful. Parents and caregivers often advocate for options that will cause less disruption to the child’s daily activities, schooling, and family life, making treatments like ravulizumab (less frequent infusions) or future at-home options like crovalimab and iptacopan especially appealing.
With more therapeutic options available, healthcare providers are increasingly involving aHUS patients in the decision-making process, especially since quality of life and personal preference play such crucial roles. Patients often express a preference for options that fit their routines, minimise travel and infusion time, and improve overall convenience. Although there are concerns that patients wishes may be overridden by doctors for other reasons.
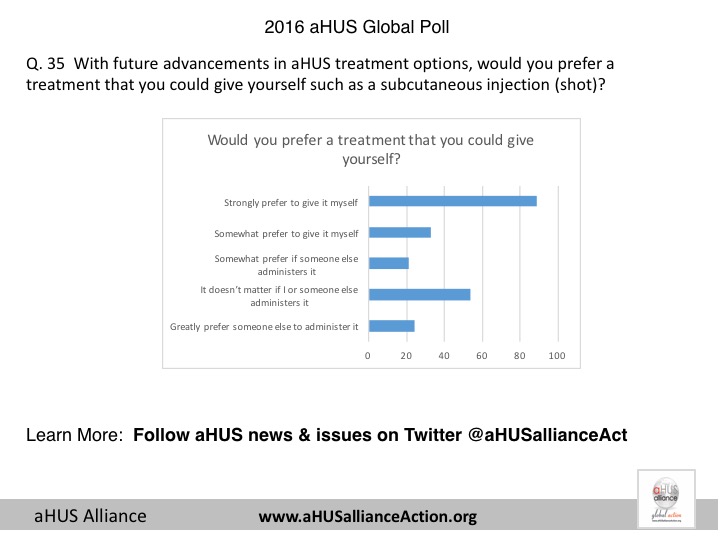
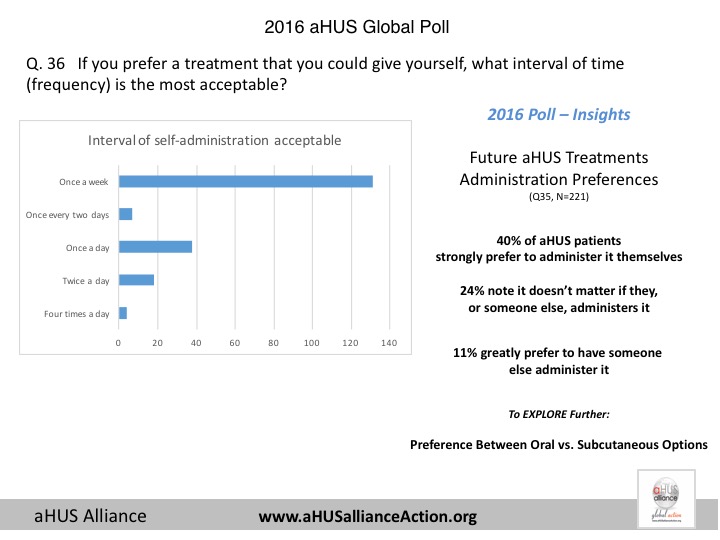
Anticipating potential choices of treatment in the future in 2016 Global Action sought patients views on locus of control of patients and the higher frequency end of treatment delivery. The graphs of results from over 200 aHUS patients globally are shown at the end of this article.
Access to newer therapies may vary by region, and insurance coverage can also impact patient choice. While in some areas patients can actively choose between eculizumab and ravulizumab, options like crovalimab and iptacopan might still be limited to trial settings or pending approval for marketing and funding.
Whilst it is great that in the mid 2020s that there is the possibility of greater choice of treatments for aHUS patients it is the highest concern of patients themselves that a treatment is also accessible and affordable for all.
What the RDD24 aHUS video tells us.
The Steven Spielberg of aHUS videos (Jeff) has produce another aHUS video for RDD24. Sixty six aHUS patients /carers starred in it*. In a few word they expressed what they…
Article No. 694
Article No. 294

