What does the internet have to say about news of change of name for aHUS?
Global Action asked it, has the name aHUS been changed. This is the answer it got.
“Currently, the name “atypical hemolytic uremic syndrome” (aHUS) has not been officially changed, but discussions about renaming or reclassifying the disease have been ongoing within the medical and research communities.
One proposed alternative, “Complement-Mediated Thrombotic Microangiopathy” (CM-TMA), reflects the disease’s underlying cause more accurately for some patients. However, these potential changes remain complex due to overlapping conditions and their distinct diagnostic and treatment needs.
Advocacy groups, including the aHUS Alliance Global Action, have expressed concerns about how a name change might impact patients, such as increased confusion or challenges in obtaining treatment. These organizations have been monitoring developments and advocating for patient inclusion in the discussions.
As of now, no official timeline or decision has been announced for adopting a new name.
For updates, aHUS-related advocacy organizations and their websites, like the aHUS Alliance Global Action or the aHUS Foundation, remain valuable resources for the community.”
We asked that if not officially changed is the new nomenclature being used by clinicians and researchers.?
“Yes, the new nomenclature for aHUS, particularly the term “Complement-Mediated Thrombotic Microangiopathy” (CM-TMA), is increasingly being used by clinicians and researchers. This shift reflects efforts to better align the terminology with the understanding of the disease’s pathophysiology, particularly its roots in complement system dysregulation.
Studies, research presentations, and clinical discussions often use CM-TMA to describe conditions that fall within the aHUS spectrum, especially when referring to complement-related mechanisms in thrombotic microangiopathies (TMAs). The term highlights the broader group of diseases with overlapping features, which aids in research and clinical clarity. For example, CM-TMA distinguishes itself from other TMAs like thrombotic thrombocytopenic purpura (TTP) or Shiga-toxin-mediated HUS (STEC-HUS), which have different etiologies and treatments.
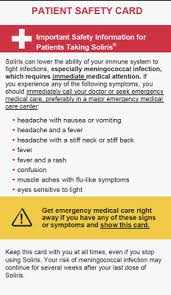
This gradual adoption in academic and medical circles is not yet universal and has created some confusion. Advocates worry that the transition lacks patient involvement and might complicate diagnostics and treatment access. However, the use of CM-TMA allows clinicians to focus on the specific complement dysregulation seen in these cases, which can guide targeted therapies such as eculizumab.”
For patients and caregivers, staying informed through advocacy organizations like the aHUS Alliance Global Action and engaging with healthcare providers is key to navigating this evolving terminology.
But the classification CM- TMA is proposed to have sub types.
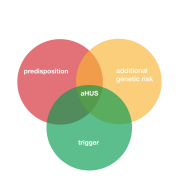
“Yes, the emerging classification of “Complement-Mediated Thrombotic Microangiopathy” (CM-TMA) includes several distinct subtypes, reflecting a more nuanced understanding of the underlying causes of complement dysregulation and its clinical presentations. The recognition of these subtypes aims to improve diagnostic accuracy and treatment strategies.
Here are the primary classifications within CM-TMA that researchers and clinicians are discussing:
1. Hereditary CM-TMA: This type is caused by genetic mutations in complement-regulating proteins such as CFH, CFI, MCP, or C3. These mutations predispose individuals to dysregulated complement activity, leading to the typical clinical features of aHUS.
2. Autoimmune CM-TMA: This involves the production of autoantibodies against complement-regulating factors, such as anti-CFH antibodies. These autoantibodies disrupt the normal regulation of the complement system and trigger thrombotic microangiopathy.
3. Secondary CM-TMA: This form is associated with external triggers such as infections, medications, pregnancy, or other systemic diseases (e.g., lupus or malignant hypertension). While these triggers activate complement pathways, the underlying genetic or immune susceptibility to complement dysregulation may still play a role.
This classification system highlights that CM-TMA encompasses a broader spectrum of diseases than what was traditionally recognized under “aHUS.” It also underscores the need for specific diagnostics to determine the root cause and guide therapy, such as complement inhibitors (e.g., eculizumab).
The adoption of these terms is gradually increasing, but as noted by advocacy groups like the aHUS Alliance Action, the transition to this nomenclature raises concerns about clarity for patients and continuity of care”
Finally where do those with no genetic mutation nor secondary cause fit it in?
For individuals diagnosed with aHUS who lack detectable genetic mutations or a clear secondary trigger, their condition typically falls into a subset of idiopathic CM-TMA (Complement-Mediated Thrombotic Microangiopathy). This classification reflects cases where the underlying cause remains unclear despite thorough testing, including genetic, autoimmune, and environmental investigations.
Characteristics of Idiopathic CM-TMA
1. No Genetic or Autoimmune Markers: These patients do not exhibit known mutations in complement-regulating genes or detectable autoantibodies, such as anti-CFH.
2. No Obvious Trigger: There is no evident secondary factor like infection, pregnancy, or systemic disease to explain complement dysregulation.
3. Similar Pathophysiology: Despite the absence of identifiable causes, these cases are presumed to involve dysregulation of the complement pathway based on clinical presentation, laboratory findings, and response to treatment with complement inhibitors (e.g., eculizumab).
Challenges in Classification
These idiopathic cases highlight gaps in our current understanding of aHUS and CM-TMA. Researchers speculate that:
• Undiscovered genetic mutations or rare polymorphisms may still be present.
• Subtle immune system anomalies or environmental interactions may contribute to disease onset.
• Diagnostic limitations may obscure the identification of secondary triggers.
Implications for Treatment and Research
Patients without identifiable mutations or triggers often benefit from complement-inhibiting therapies, suggesting that complement dysregulation is still a driving factor. Their inclusion under CM-TMA acknowledges the broader spectrum of complement-mediated diseases while encouraging ongoing research into unexplained cases”
This subset demonstrates the need for further refinement in classification and diagnostic tools to provide clarity and ensure targeted, effective treatment.
So that is what the internet has to say about the new name for aHUS. Although not official it is already happening in a seeping inundation kind of way. It is not known when an “official” decision is to be made or even the timeline for its implementation. Whether there is ever going to be an official implementation stage even.
It may be pandering to the enquirer but the internet sees patient groups such as aHUS alliance Global Action as providing insights into the evolving change of name and its diagnostic considerations for aHUS.
Having said that the internet does not always provide the full answer on the proposed change of name , missing idiopathic or Non – Genetic – TMA and using Heredity CM- TMA when it’s reclassification name is Genetic CM-TMA and would include sporadic genetic CM-TMA cases too.
Article No.697
Previous articles on aHUS name change

Out with old in with the new- not quite just yet
On the 10th anniversary of international aHUS awareness day it is timely to raise awareness that the old term aHUS is on its last legs and is to be replaced.…

Is aHUS’ end nigh? It is now!
Nearly five years ago Global Action asked the question “ Is aHUS’s end nigh ?” In a trilogy of articles. ( click HERE for the first of the 3) Not…