Since its inception in 2008, and celebrated annually on the last day of February, world Rare Disease Day has been an opportunity to provide information and advocacy for and about the rare disease community. That makes this month a perfect time for us to take action with another update of newly released aHUS-specific publications added to the ‘aHUS Virtual Library’ hosted by the aHUS Alliance Global Action team.
Reasons to Keep Pace with aHUS Research
Actually, there are many. You scan the internet for information and reviews often, whether considering purchase of a vehicle or searching for a home repair service – so why not also employ that dedication for health information as well? Whether you’re in the medical field or a patient, context to integrate and utilize that new knowledge is vital.
Thrombotic microangiopathies (TMA) include a range of medical conditions where blood clots form in capillaries and small arteries around the body and cause organ damage. Atypical HUS is one cause of TMA activity, but others are infection, pregnancy, certain medications, some autoimmune or connective tissue diseases, surgeries, and more.
And therein lies both the problem as well as the pathways to advancement. If the root cause (or triggers) can be better identified, tailored treatment and targeted disease management can offer better patient outcomes.
Treatment needs to focus on managing the underlying cause or causes (etiology) of TMA activity, and clearer names (nomenclature) that can indicate the best treatment for an individual patient. Plasma exchange, combined with immune suppression, can be an effective therapy for those TMA patients diagnosed with TTP but patients diagnosed with aHUS may be more effectively treated with a complement inhibitor. While an inability to control or regulate the body’s complement system affects the majority of aHUS patients (complement-mediated TMA or cmTMA,c-TMA), those with DGKE mutations often do not respond well to complement inhibitors because their disease mechanism is independent of complement activation. Other aHUS patients may have genetic test results indicating C5 polymorphisms, which are resistant to complement inhibitors.
From December 2024 through mid-February 2025, we’ve added about three dozen pieces of research to our ‘New Research’ scroll. As usual, we’ve provided context so our readers gain insight into how these publications have potential to affect aHUS patients’ diagnosis and treatment. Here are a few:
Different Treatments may be More (or less) Effective
Managing care for atypical HUS patients is not a ‘one size fits all’ scenario. Each case of aHUS is unique in terms of severity, organs affected, or duration of aHUS activity. While a patient diagnosed with atypical HUS exhibits the effects of TMA microclots which affect organ function, it’s key to repeat that some subtypes of aHUS may not respond well to complement inhibitors. On top of that, many nations have rare disease policies which either: regulate or restrict physician access to drugs which are high cost, offer complement inhibitors but limit their duration, or patients can access such drugs but without reimbursement or insurance mechanisms to help cover their cost.
So what happens to patient health, given the high costs and specialized nature of complement inhibitors, with availability is often limited in low- and middle-income countries? How are aHUS patient outcomes affected, given this harsh reality one can infer that these therapies are accessible in a minority of the world’s nations? Let’s look at patient outcomes for TMA, which of course includes people with the broad-ranging diagnosis ‘atypical HUS’.
Kaname S et al. Outcomes in patients with thrombotic microangiopathy associated with a trigger following plasma exchange: A systematic literature review. Transfus Apher Sci, Vol 64, Issue 1, 2025,104048, doi.org/10.1016/j.transci.2024.104048.
“Patients with trigger-associated TMA may experience a substantial burden in terms of mortality, relapse, and progression to CKD and ESRD following PE, leading to increased healthcare resource utilization.” and “In patients with aHUS, PE effectiveness is generally poor, varies by genotype, and has only been shown to be relatively effective in patients with pathogenic mutations in genes that code for circulating complement regulators (such as CFH). For example, in patients with pathogenic mutations in the complement-associated CFI gene, PE/PI was associated with a 25 % remission rate.”
van Doorn DPC et al. Etiology and Outcomes of Kidney-Limited and Systemic Thrombotic Microangiopathy. Mod Pathol. 2024 Dec 16;38(4):100690. doi: 10.1016/j.modpat.2024.100690
“Patients with TMA should be classified according to etiology to indicate targets for treatment at the earliest possible stage of disease, having an impact on prognosis. Kidney-limited TMA, although often overlooked, appeared common along the diverse TMAs, including complement-mediated (C-)TMA.” and “Kidney-limited TMA is common along diverse TMAs and is found in 57%, 48%, and 79% of patients with definite C-TMA, probable C-TMA, and nC-TMA, respectively.”
Pregnancy & aHUS
Athough we’ve added a handful of recent publications to our virtual library’s scroll on the topic of aHUS and pregnancy, here are two ‘don’t miss’ publications. The first showcases the rare occurrence where the title and publication indicates quite clearly why we’ve chosen to highlight this article on pregnancy-associated hemolytic uremic syndrome (pa-HUS). Unfortunately for aHUS advocates and patients, a full text or ‘open access’ option is not readily available.
Al Mashikas, J et al. The Kidney of the Critically Ill Pregnant Woman (Book, Chap 8). Critical Care in Obstetrics: HUS in Pregnancy. Academic Press ISBN 9780443214738. 2025, Pages 85-91. https://doi.org/10.1016/B978-0-443-21473-8.00019-7.
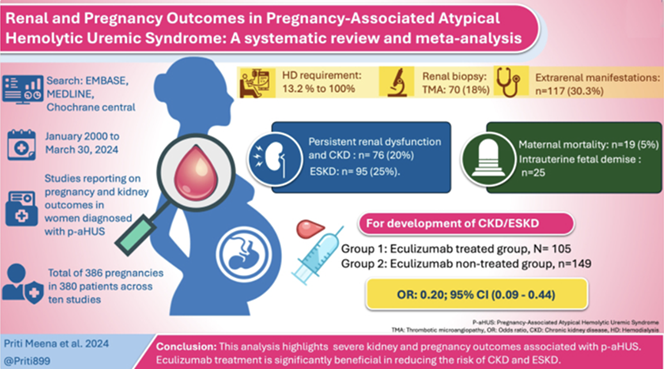
Looking for all the latest findings on atypical HUS and pregnancy? Here it is, with a wealth of information and insights gleaned from 10 studies which encompassed 386 pregnancies in 380 patients. A great graphic abstract from lead author Dr Priti Meena (India) showcases this work, which covers aspects of kidney function/damage as well as pregnancy outcomes for women with aHUS.
Meena P et al. Kidney and pregnancy outcomes in pregnancy-associated atypical hemolytic uremic syndrome: A systematic review and meta-analysis. Medicine (Baltimore). 2025 Jan 31;104(5):e41403. doi: 10.1097/MD.0000000000041403.
Nation-Specific Research: of Benefit to All
Given the many gray areas and knowledge gaps throughout information regarding atypical HUS, it’s really something to celebrate when a group of aHUS experts published a ‘consensus statement’. From diagnosing aHUS apart from other syndromes of thrombotic microangiopathy to recommendations for treatment and disease management, this Brazilian consensus statement has high value for aHUS patients and medical providers worldwide. We’re pleased to note that the aHUS Alliance Global Action team hosts the resource SHUa: em Português, as a Portuguese language asset created in collaboration with aHUS Brasil. The driving force behind aHUS Brasil is its founder Pamela Notario, who is a valued member of the global Atypical HUS Community Advisory Board (CAB).
Vaisbich et al. Recommendations for diagnosis and treatment of Atypical Hemolytic Uremic Syndrome (aHUS): an expert consensus statement from the Rare Diseases Committee of the Brazilian Society of Nephrology (COMDORA-SBN). J Bras Nefrol. 2025 Apr-Jun;47(2):e20240087. doi: 10.1590/2175-8239-JBN-2024-0087en.
Indicative of diagnostic dilemmas faced by personnel in ‘emergency medicine’ roles, it’s not so much that it’s difficult to scan lab test results to see if problems exist with indicators such as abnormal red blood cell values or a decline in platelet counts. What is hard to differentiate is the root (etiology) of what might be causing deterioration of patient health, since such labs are common indices for a wide number of medical conditions.
As noted by the authors of this publication, “Diagnosing a TMA syndrome, causal differentiation and treatment require specialist knowledge that is not always available in acute and emergency medicine. Many differential diagnoses and examinations are usually necessary to make a correct diagnosis. Therefore, a standardized diagnostic algorithm is helpful for early diagnosis and treatment initiation.”
Potthoff SA. Thrombopenie und hämolytische Anämie in der Akut- und Notfallmedizin : Detaillierter Blick auf thrombotische Mikroangiopathien [Thrombopenia and hemolytic anemia in acute and emergency medicine : Detailed view at thrombotic microangiopathies]. Inn Med (Heidelb). 2025 Jan;66(1):64-81. German. doi: 10.1007/s00108-024-01835-8. Epub 2025 Jan 22. PMID: 39841188.
The original is written in German, and unfortunately unavailable as full text or in ‘Open Access’ versions. Germany has an active patient organization called Germany Selbsthilfegruppe MPGN Und aHUS E.V (www.ahus-selbsthilfe.de), and we’re pleased to note that Christiane Mockenhaupt as one of their founders is a valued member of the global Atypical HUS Community Advisory Board (CAB).
Over 1,400 aHUS-specific publications are cataloged within
A ‘Virtual Library’ of aHUS-specific Research – What is that?
Often publications with advancements and insights into this very rare disease are scattered across medical journals related to nephrology and hematology specialties, but atypical HUS information can be found under varied terms and across specialty areas. That’s where we come in, since as aHUS patients and family caregivers ourselves we have a vested interest in staying up-to-date with current research. It’s likely that other families affected by aHUS may wish to key into a specific topic, so to aid navigation of our ‘Research and Publications’ page we’ve not only categorized entries but also have added links to jump to each Scroll (topic section) to speed your search.
Research articles about atypical HUS are listed within our website on topic-specific lists within our Info Centre, where you can see a list for “New Research” which are then also listed by category. Scroll topic categories are: New Research, Critical Care, Diagnosis, Treatment, Discontinuing Treatment/Relapse, Thrombotic Microangiopathy (TMA), Extra Renal (Effects on Organs other than Kidneys), Pregnancy, Transplants, Genetics, Complement, Secondary aHUS, Triggers, Research in Specific Nations, Case Studies, Patient Registries: Publications, Drug Discovery/Research, Summary Articles/Literature Reviews, Consensus Documents/Guidelines, and Varied Topics.
(Note: All entries from the ‘New Research’ scroll additionally are cross-listed at the start of each specific topic. While this ‘library’ has grown to over 1,400 unique publications, it results in about 1800 dual entries – such as a study that examines mutation impact on disease management, and thus listed on both Genetics and Treatment scrolls.)
Visit our ‘virtual library’ of over 1,400 publications specific to aHUS
by clicking this link: Atypical HUS Research & Publications
Keeping Pace with Advancements: Are you ‘aHUS Aware’?
The aHUS Alliance Global Action team encourages researchers to release their studies and publications in full text versions, with Open Access to facilitate sharing knowledge. Additionally, we welcome and applaud those individuals and groups who include “Plain Language Versions” as part of their publication’s Supplementary Materials.
Are you staying current with aHUS research & News?
We invite you to subscribe to our free newsletter, The aHUS Global Advocate
For More about our Newsletter & reasons to Stay Connected
Click Here to Sign Up to receive the Newsletter

