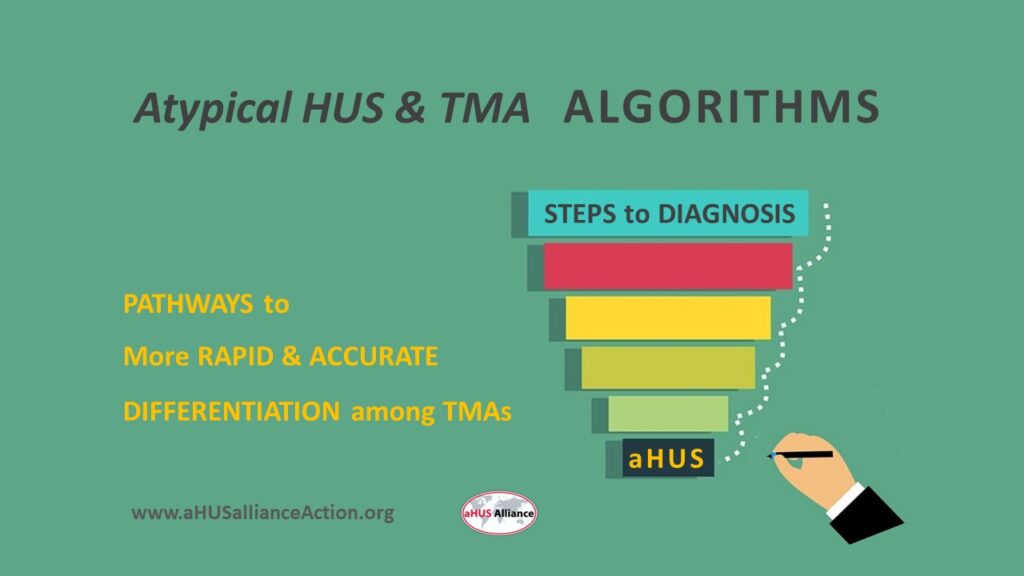
What if there was a set of actions, decision points, and guidance steps to help physicians determine whether a patient had atypical HUS or some other medical condition? Wouldn’t that be likely to provide more rapid diagnosis leading to better outcomes?
Actually, such tools do exist – they’re called algorithms. In simple terms, an algorithm is simply a set of defined steps used to solve a specific problem or task. Atypical HUS is a ‘diagnosis of exclusion’, meaning that medical teams must go through the processes which rule out medical conditions with similar presentations – until all that’s left is the option for diagnosis of atypical Hemolytic Uremic Syndrome.
While it’s heartening that many aHUS patients receive a rapid and accurate diagnosis, a large percentage of patients report their journey to diagnosis to be long and challenging to navigate. Once reaching specialist care, 47% of aHUS patients received a diagnosis within 7 days or less but 13% remained undiagnosed or misdiagnosed for 365 days or longer. The diagnostic experience for adults it took longer, with only 37% of patients being diagnosed in 7 days or less (Source: aHUS Alliance Global Action poll: Report 3 from our 2021 survey data on patient diagnostic experiences).
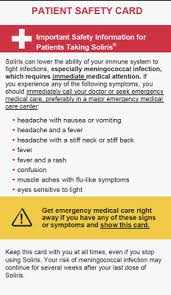
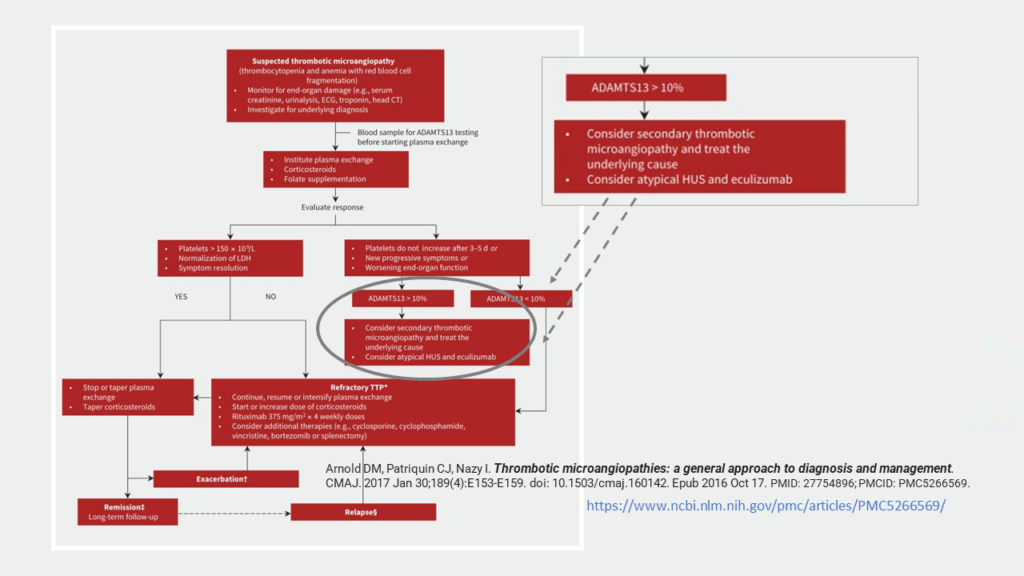
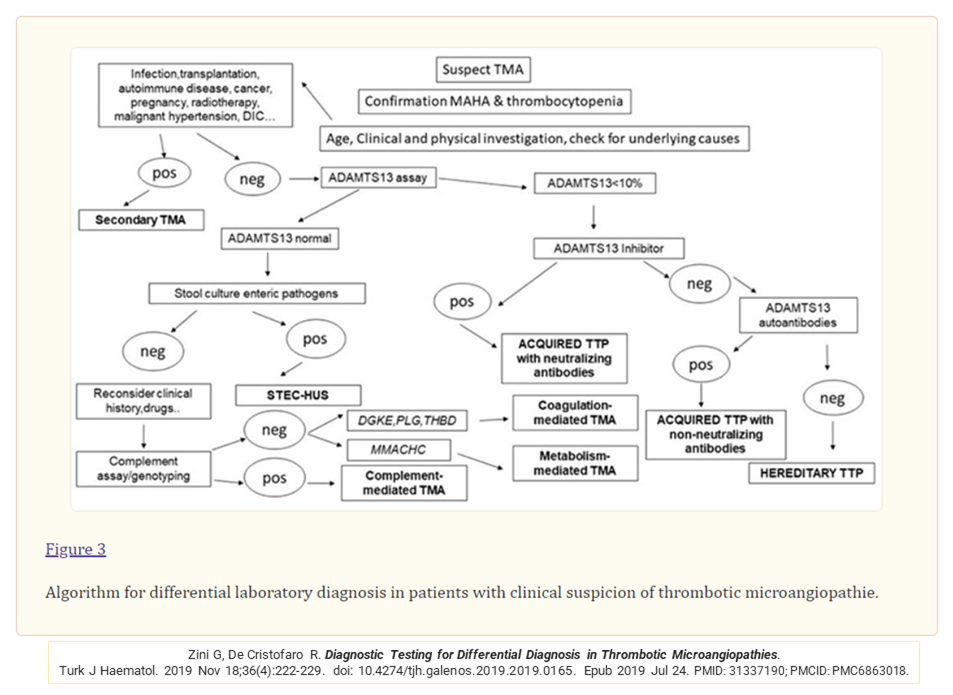
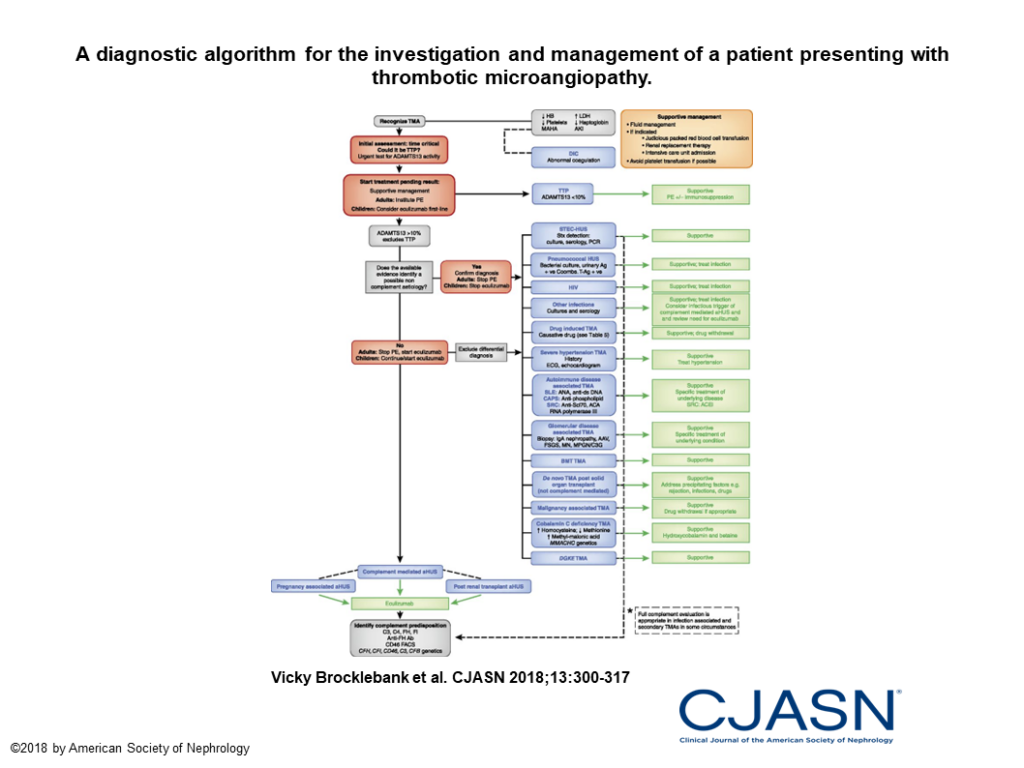
What may surprise you is that while several aHUS/TMA diagnostic algorithms have been published over the past few years, but they seem to lack visibility. You’ll note there’s a common initial step in these problem-solving flow charts for testing of ADAMTS-13 levels, an important determination in distinguishing atypical HUS apart from TTP or other syndromes of thrombotic microangiopathy.
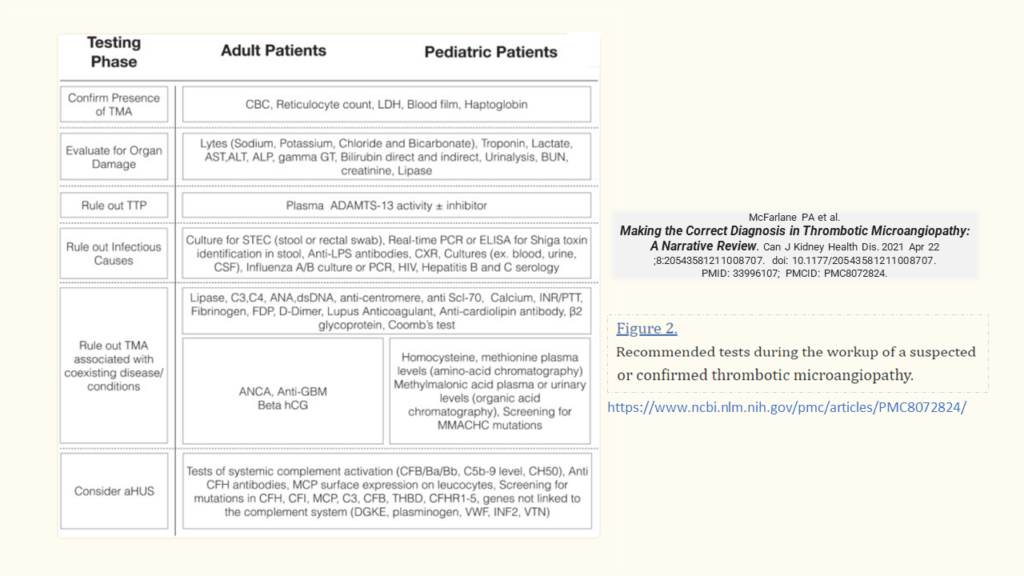
Here’s an example in which it’s readily seen regarding specific tests which can help guide the diagnostic process, and which also shows aHUS at the bottom of the chart (McFarlane et al. 2021 Making the Correct Diagnosis in Thrombotic Microangiopathy: A Narrative Review)
Diagnostic algorithms have existed for several years. Here’s one example that was available online in October 2016, covering differential diagnoses of thrombotic microangiopathies and diagnostic tests. Arnold DM et al. Thrombotic microangiopathies: a general approach to diagnosis and management.
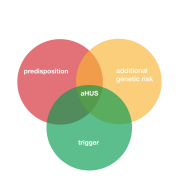
Acquired or Hereditary? As the term ‘acquired’ indicates, some forms of TMAs are triggered by events such as with pregnancy-triggered aHUS, while ‘hereditary’ refers to a genetic background or mutation passed down among family members. Here’s a flowchart type of algorithm which includes this aspect. Zini and De Cristofaro, 2019. Diagnostic Testing for Differential Diagnosis in Thrombotic Microangiopathies. (See also Table 1: TMA Causes)
There’s a wealth of information within publications which contain diagnostic algorithms. Case in point, the Brocklebank et al. 2018 publication Thrombotic Microangiopathy and the Kidney. Among its informative images is Figure 3: Thrombotic microangiopathies are classified into: Inherited or acquired primary; secondary; or infection associated TMAs.
People experiencing their initial onset of atypical HUS often escalate to acute care, with 31% of patients polled reporting their health status as ‘life threatening’ and 32% designating that status reached a critical condition level. (Source: aHUS Alliance Global Action poll: Report 3 from our 2021 survey data on patient diagnostic experiences).
Here are two articles on diagnosis of aHUS apart from similar conditions of thrombotic microangiopathy. Note that both have algorithms for problem-solving for intensivists and urgent care personeel to distinguish among types of TMAs.
Azoulay E et al. Expert Statements on the Standard of Care in Critically Ill Adult Patients With Atypical Hemolytic Uremic Syndrome. Chest. 2017 Aug;152(2):424-434. doi: 10.1016/j.chest.2017.03.055. Epub 2017 Apr 23. PMID: 28442312.
Vincent JL et al. Thrombocytopenia in the ICU: disseminated intravascular coagulation and thrombotic microangiopathies-what intensivists need to know. Crit Care. 2018 Jun 13;22(1):158. doi: 10.1186/s13054-018-2073-2. PMID: 29895296; PMCID: PMC5998546.
Perplexing Points to Ponder
Volunteers of the aHUS Alliance Global Action team, as an international advocacy group composed of patients and caregivers, are aware that there are flowcharts to assist with aHUS/TMA diagnosis.
Rapid and accurate diagnosis is vital to promote better patient outcomes, with treatment-naive patients either enrolled in clinical trials, or quickly moving to appropriate treatment plans. Multidisciplinary care teams (MDTs) can diagnose and guide the complex care of patients presenting with multiorgan involvement common for syndromes of thrombotic microangiopathy.
So…. Why isn’t there more emphasis on establishing MDTs with more visibility for, and MedEd engagement with, TMA algorithms which include aHUS diagnostic pathways?
About the Author:
Linda Burke is a Trustee of the non-profit aHUS Alliance Global Action, and a founding member of the global aHUS Community Advisory Board. She creates visual and written content to highlight aHUS topics and issues, to include contributions to publications noted below.
Together we appreciate the efforts of clinician researchers around the world who collaborate with, and value, aHUS patient voices and advocacy efforts.
Raina R, Grewal MK, Radhakrishnan Y, Tatineni V, DeCoy M, Burke LL, Bagga A. Optimal management of atypical hemolytic uremic disease: challenges and solutions. Int J Nephrol Renovasc Dis. 2019 Sep 4;12:183-204. doi: 10.2147/IJNRD.S215370. PMID: 31564951; PMCID: PMC6732511.
Yerigeri K, Kadatane S, Mongan K, Boyer O, Burke LLG, Sethi SK, Licht C, Raina R. Atypical Hemolytic-Uremic Syndrome: Genetic Basis, Clinical Manifestations, and a Multidisciplinary Approach to Management. J Multidiscip Healthc. 2023 Aug 4;16:2233-2249. doi: 10.2147/JMDH.S245620. PMID: 37560408; PMCID: PMC10408684.
Burke L, Sethi SK, Boyer O, Licht C, McCulloch M, Shah R, Luyckx VA, Raina R. Voice of a caregiver: call for action for multidisciplinary teams in the care for children with atypical hemolytic uremic syndrome. Pediatr Nephrol. 2023 Oct 2. doi: 10.1007/s00467-023-06158-8. PMID: 37782345.