The aHUS Alliance is pleased to present this informal interview with Dr. Gianluigi Ardissino, a clinician and researcher affiliated with Centro per la Cura e lo Studio della Sindrome Emolitico Uremica (Centro SEU, Center for HUS Control) and Expert Centre in Milan Italy. Part of our ongoing aHUS Alliance series titled Perspectives in aHUS, Dr. Ardissino discusses the interface with HUS and TMA to provide insight into how these topics are highly relevant and of great interest to us. We appreciate his impressive array of aHUS articles and collaborative research, and offer our deep thanks to Dr. Ardissino for his commitment to patients and dedication to explore advancements in treatment options. Grazie!
Question 1
Given your many interests as an aHUS investigator and clinician, what is your current professional focus?
As a clinician most of my time is devoted to patients’ care. By doing this and paying attention to the needs of patients, I often come up with interesting observations which can be focused and documented to later become an investigation worth being shared. This was the case of the study regarding discontinuation of eculizumab treatment in aHUS for which the rational was to improve the patient’s quality of life, to protect them from potentially serious infections, to prevent sensitization to the drug and of course to make the treatment sustainable. We now have a great drug for treating aHUS but we still need to learn (and teach) how best to use it. A specific responsibility and mission of doctors is the care of patients, otherwise we have to follow the indications of the industry. The same holds true for tailored eculizumab treatment for those patients who cannot discontinue the treatment due to severe renal impairment, kidney transplant, previous relapse or unwillingness to discontinue eculizumab infusions. Tailored eculizumab therapy occurs when we individualize the treatment schedule based on complement suppression that is actually needed. None of my patients is receiving eculizumab every 14 days but rather every 21 days (35% of them) or every 28 days (65% of them). This has reduced the burden of treatment quite a lot, improving patient quality of life while cutting costs. I just presented our results at the 6th International Conference on HUS and Related Disorders : out of 44 patients followed for a cumulative observation period of > 100 years we did not experience a single relapse.
2. Much remains to be learned about aHUS and related diseases. Where have we made the most progress and what areas are largely unexplored?
Eculizumab has dramatically changed the outcome for aHUS patients, and this is something I have never experienced for any other disease since my graduation in 1985. This is a goal reached ! Now among the most important unmet needs, from the clinical viewpoint, is Bone Marrow Transplant-Related TMA (post-BMT TMA). This condition is common among patients undergoing transplantation, but the disease does not respond to eculizumab very well although it looks very similar (and some doctors consider it a type of aHUS). Another area to concentrate effort is the need to promote early recognition and early diagnosis of aHUS. We have demonstrated quite clearly that early treatment is associated with better outcome as to response rate, level of residual renal function, and time to obtain full recovery. This is particularly relevant for aHUS triggered by partum which, if unrecognized and untreated, can leave behind a child without the mother or with a mother on dialysis. Much remains to be done in collaboration with obstetricians on this area.
3. What might be the ‘next big thing’ in the near future for regarding advancements related to aHUS?
I think it may be a new drug to maintain remission, administered subcutaneously maybe every other month or even less often. This exists currently as an investigational drug, but it remains to be tested and go through the clinical trial progress. It might be available in the near future, within several months or very few years. It is not easy to predict what comes next. I remind you that nobody had predicted the availability of eculizumab when first was introduced as a therapeutic option for aHUS treatment in 2009. It was only an intuition of a pediatric nephrologist from Innsbruck. Science is also intuitive and intuitions cannot be predicted.
4. What else might you feel important, which you’d like to share with others?
You mainly deal with aHUS but do not forget typical HUS (called STEC-HUS, D+HUS, eHUS) which has a similar presentation that may result in diagnostic confusion, mistaking one condition for the other. This disease mainly affects children and is still burdened by a mortality rate much higher than aHUS. There are some therapeutic opportunities which, in Milano, have lowered the patient mortality rate to 0 (zero). I have recently published in “Pediatrics” an article with the results of this investigation, perhaps the most important investigation I have ever published (if importance is measured in terms of life-saving potential). This therapeutic opportunity is poorly known and not widely applied, perhaps because the treatment is very cheap and not backed by a pharmaceutical company advocating its use. Perhaps this is where academia and the government should focus attention and efforts, since nobody else would invest resources to develop and promote therapies that are not going to yield profits.
We welcome your questions and feedback, and we invite other clinicians, researchers, and investigational teams to contact us regarding interest in aHUS Perspective interviews.
We thank Dr. Ardissino, Director of the Center for HUS Prevention, Control and Management at the Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, IT for his generous participation with this interview.
Connect with the aHUS Alliance: info@aHUSallianceAction.org
June 2017
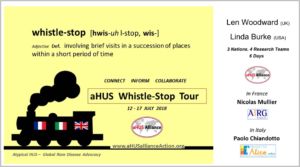
aHUS Alliance visit to Centro SEU (July 2018)
Whistle-Stop Tour of 4 aHUS Centers in the EU: Visits to Three Nations in 6 days
Click below to READ

