Article No. 299
1 December 2019
Currently some challenge is taking place on the terms used to describe diseases in which TMA , Thrombotic Microangiopathy, is a key factor, and aHUS is one of those terms.
Accepted use of the term aHUS took a long time to arrive at.
No one knows how long the disease aHUS has existed. Complement has been around for millions of years.
In the early 20th century aHUS it would have fallen within the scope of what became known as Moschcowitz Syndrome. Named after the clinician Eli Moschcowitz from USA who identified the symptoms of thrombosis, low platelets and purpura ( bruising) in 1924.
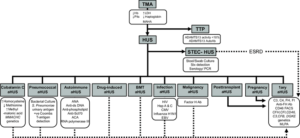
The name was then changed to Thrombotic Thrombocytopenic Purpura (TTP) emphasising the symptoms of a very serious disease. TTP remained the name until Prof Symmers coined the term TMA ,Thrombotic Microangiopathy, in 1952 which made TTP a more specific term , and again in 1955 Von Gasser came up with Hemolytic Uremic Syndromes ( HUS ) which differentiated it from TTP. But such was the overlap the diseases were commonly known as HUS /TTP for the next few decades.
Although Von Gasser had used “syndromes” to suggest there were at least two forms of HUS, the term “atypical” did not appear until 1965 in the Central African Journal of Medicine, when Barnard and Kibel in a study of 11 HUS cases in children described one of the cases as “atypical” as it had not been preceded by diarrhoea as had the other ten. Those 10 cases were thought to be result of something like a strain of e. Coli , although it was just a theory at that time. The name aHUS did not result from that article.
It was an article in 1993 which was coauthored by Prof. Martin Barrett from Great Ormond Street Hospital, London, which is credited with first using “atypical Hemolytic-Uremic Syndrome”. Although even that group felt it safer to insert in brackets after “atypical” – “non diarrhoeal associated”. That article even asserted that some of the children included in the study might have genetic causes of their aHUS.
From 1993 it took some time for the term aHUS to catch on. aHUS is not mentioned in the 1998 study by Warwicker /Goodship in which the first aHUS disease predisposing genetic mutation in Complement was found and reported.
It was more likely that “inherited” or “familial” HUS would be used. Or even “sporadic “ if no infection nor family link could be found.
By the time the Foundation for Children with atypical HUS – (now the Foundation for atypical HUS) was formed in the USA in 2001 by Bill and Cheryl Biermann, the term aHUS was clearly in use. Although in clinical publications of the time it was still likely to be referred to as atypical “and familial HUS”.
Through those aHUS advocacy pioneers, and their websites, an awareness of aHUS was built up within the patient community; mirroring a similar growth of use and acceptance in the clinical community.
By 2007 Alexion was also using the term aHUS when it was getting ready to trial eculizumab as a treatment for the disease.
At the KDIGO Controversy Conference in 2015 the classification Primary and Secondary aHUS was agreed to begin a differentiation, but keeping aHUS as the main term.
The Campistol Group in Spain had seen a TMA spectrum as something like this:
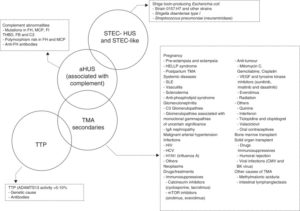
Keeping aHUS , pbut regarding the secondary aHUS as TMA with an overlap with both TTP and aHUS.
Vicky Brocklebank’ s group at Newcastle continued a re-categorisation of Primary and Secondary TMAs into inherited or acquired susceptibility factors in 2017. Seeing it like this
As did the Craig Gordon’s Group In Boston, in the same year, who also saw primary and secondary TMA categories.
In both the above classifications the term aHUS is noticeable by its absence.
By 2019 after 95 years of name changes we have arrived at a point where aHUS is known and used ubiquitously.
So why are there are rumblings about it and a movement building to replace it?
What the implications are for patients and patient organisations ,if or when aHUS is replaced, will be addressed in part 2 and 3 of “aHUS is its end really nigh”.

