Recently a novel article about complement inhibitor treatment discontinuation was published. Novel because of the research method used to produce its results.
A qualitative study based on interviews with ten international aHUS experts who agreed to participate out of 25 who were invited.
Treatment discontinuation in adults with atypical hemolytic uremic syndrome (aHUS): a qualitative study of international experts’ perspectives with associated cost-consequence analysis
As this study was confined to adult patients only , seven declined as their experience was of paediatric patients only. The other 8 did not reply.
None of the doctors participating were named.
The research study was funded by Astra Zeneca Alexion. The full article can read HERE.
In structured interviews lasting on average about 30 minutes each, participants were asked to speak about their experience of managing straightforward patient cases, and then complicated cases. Followed by how they monitored and managed relapses and what guided treatment discontinuation decisions.
The resultant output from the around five hours recorded chat was analysed and categorised to establish themes.
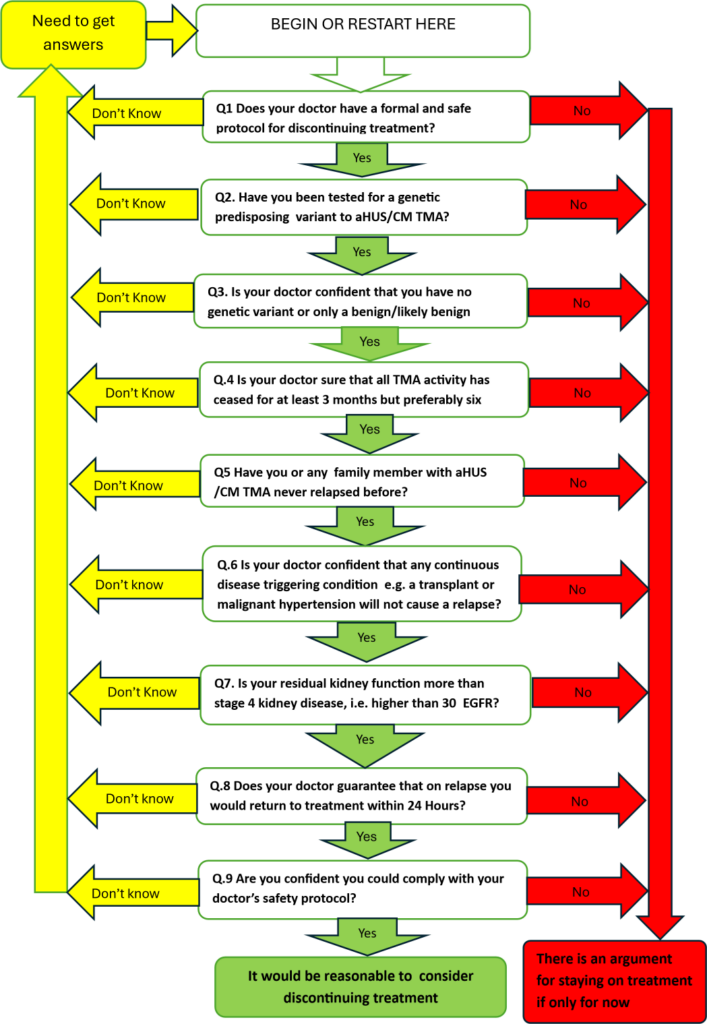
From it a decision tree was conceptualised on continuing and discontinuing treatment. It is a logical representation.
What then follows is a description of the views of the participating doctors about:
- Concerns and experience by doctors
- high risk v low risk groups
- funding for monitoring and re-treatment
- patient preference and adherence
Personal concerns and experience of doctors led to two distinct doctor groups. Firstly those who would never and then those who would consider discontinuing treatment. (Global Action has found that is much the same as patients feel).
In the high risk v low risk views of participant a list of ten factors in order of mentions by the doctors is given, for example there was one mention of extra renal manifestations, up to ten mentioning the improvement in kidney function. (The factors thought important mapped to those used in Global Action’s model for discontinuation decision making ( see below) and its background narrative).
Patient preference surrounded how comfortable doctors thought their patients were about stopping treatment (they thought the majority were) and how prepared they would be to follow and adhere to any monitoring guidelines. (Again Global Action has identified preference to discontinue by some patients if not as high a proportion as doctors think. Willingness to adhere to discontinuing monitoring protocols is a question it is included in its discontinuing treatment model).
Funding and monitoring views of doctors revealed a third party constraint to the discontinuation of treatment process. Paying for monitoring tests and having preauthorised access funding is something that is not readily accepted by payers. (Global Action supports patients unwillingness to withdraw from treatment without a rapid return to care pathway. Such monitoring costs should be netted off potential overall drug cost savings. Whether treatment is privately or publicly funded. Global Action has reported frequently on the potential savings from deploying complement inhibitors when needed for as long as is needed).
This article confines itself to the first year of treatment and not the long term . (Global Action has identified that a long term view will be needed in the long term).
This investigation by a world leading investigator and based on input from international aHUS experts has shown that doctors, and patients as represented by Global Action mirror each other’s thoughts about the practicalities and safety of the same decision to stop, or not to stop, complement inhibitor treatment.
There may not be agreement on everything by clinicians as Global Action has pointed in its research on the topic of discontinuation of treatment , but one final opinion which Global Action has previously expressed and this is also stated in this study. Our study argues for an international consensus conference to explore issues surrounding aHUS treatment duration.
Global Action would add to that including the patient voice using a trusted informed patient organisation
Article No 703

TO STOP OR NOT TO STOP – THAT IS THE QUESTION?
You have had aHUS. The type of aHUS caused by uncontrolled complement, not the other type. You got access to a complement inhibitor. It WORKED. You tolerated the drug. Your…
AN aHUS PATIENT’S TREATMENT DISCONTINUATION MODEL
Without any further comment here is the model mentioned in the previous article ( which if you have not already seen can be read HERE ). Have a go at…

