
Traveling for work or pleasure needs an extra bit of preparation for those people diagnosed with atypical HUS. By planning well in advance most people can travel and still maintain their treatment schedule to ‘stay on track’, whether to ensure their return to improved health or to maintain their level of wellness. Check early with your medical team and those engaged in all areas of your aHUS treatment plans, to include specialists and treatment providers (such as infusion or dialysis centers). People in the acute phase of illness or switching treatment regimens will likely be informed by their medical team to delay travel plans until their health and care plans achieve stability.
Let’s look at some travel information and tips for aHUS patients, suitable for either domestic or international travel, then consider special considerations for different types of aHUS patient profiles.
Dialysis & Travel
There are some common scenarios and situations within and across the spectrum of aHUS patient subsets, to include those requiring dialysis. People with dialysis needs should check with their providers and ask about pre-planning needs such as availability of dialysis centers on their travel itinerary. Common questions and their answers might center on dialysis modality, clinical settings, and information/supplies needed to prepare for travel plans. Online tools and information can give people needing dialysis a head start regarding considerations for talks with their medical team and for travel planning. There many resources to consider, and be sure to look at nation-specific sources, but here are three solid references to begin your considerations:
You can Travel with Dialysis: Start Here (National Kidney Foundation)
Traveling Outside of the U.S. on Dialysis (DaVita)
Dialysis Patient Travel Tips (NonProfit, Dialysis Patients Citizens Information Center)
Travel & Infusions: Plan ahead!
Some people using complement inhibitors, either on a two-week eculizumab or eight-week ravulizumab infusion schedule, simply need to inform their care teams of short term travel plans. That step is important, even if the journey is within your own nation and only for a brief travel period. It’s better to alert your medical team to upcoming travel than to find oneself in an unexpected situation which might negatively impact your health or disrupt your treatment schedule before or after your trip. Whether it’s travel for holiday or work, let your care team know of upcoming travel as soon as you book your trip dates and destinations. Make sure you have your Patient Safety Card, which provides vital information regarding complement drug inhibiting the ability of the immune system to fight infections such as those caused by encapsulated bacteria (like Haemophilus influenzae or certain Streptococcus strains) , and especially with patients’ risk for life-threatening meningococcal infection. For people who have discontinued eculizumab or ravulizumab, know that those risks still exist for several months after stopping those therapies so check with your medical team.
Travel Ready: Be Prepared & Carry Medical Documentation
Checking in early with your medical team is especially important to do if you’re traveling abroad to other nations, as it’s likely that a visit with a Travel Medicine/Infectious Disease specialist will be recommended for international travel. What is travel medicine? It’s a specialized look at your specific medical profile and needs in order to help avoid or reduce environmental risks and exposure to infectious diseases. Expects questions about travel dates, nations, and regions you plan to visit. Yes, there may health alerts for different regions of a single nation. An example would be a region within a nation where malaria-carrying mosquitos are common, while an urban area within that same country may not be under the same precaution. Time to be spent in a nation matters, as does whether most of your visit will occur in rural zones or city environments. A travel medicine specialist may have you forgo the malaria vaccination in favor of preventive pills for the few days you might be traveling through a high risk area. For patients on dialysis, plasma therapies, or treated with a complement inhibitor check with your medical team about: ‘live vs killed’ vaccines and regarding optimal timing of vaccine administration around treatment appointments.
If you or a family member have been diagnosed with atypical hemolytic uremic syndrome, there’s an additional level of concern regarding recurrence. Atypical HUS episodes can happen unpredictably and can cause severe damage to the kidneys and other vital organs. If you’re an aHUS patient who has discontinued treatment, or are planning to do so, part of that discussion should include ways to monitor your health. That may have included utilizing at-home urine test strips as an early indicator of blood cell hemolysis to indicate seeking immediate medical care and lab tests. If so, some urine test strips may be more ‘travel ready’ in terms of packaging and some even offer a smart phone app (one example, Diagnox brand strips*).
If you’re just traveling to another region in your nation, it’s still a good idea to bring along your travel folder. Since atypical HUS affects only a handful of patients (2 to 9) per million, most emergency care physicians would suspect the more common ‘hemolytic uremic syndrome’ or HUS, an infection most commonly caused by E. coli bacteria. There’s no single test to diagnose atypical HUS apart from other medical conditions, and their treatment isn’t the same, so if you’re unwell while traveling it’s helpful to carry documents from your medical team that clearly note your diagnosis of aHUS.
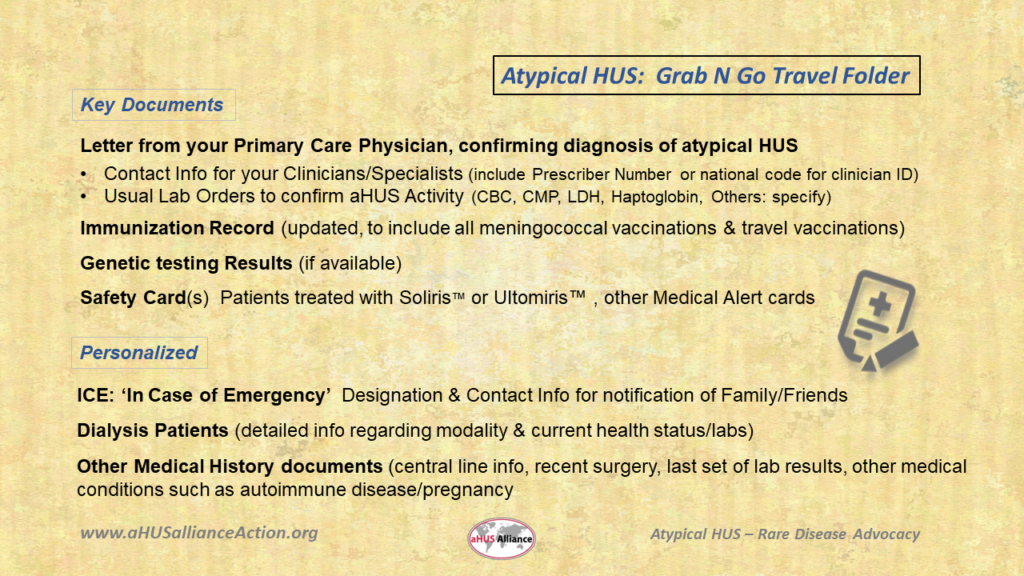
Grab N Go: aHUS Travel Folder Even if you’re simply traveling out of town for a few days, it’s still a good idea to carry medical information that documents your aHUS diagnosis. If you feel unwell away from home and seek professional medical advice, it’s sensible to provide them a firm starting point given this condition is so rare.
Food & Water: Safety vs Risk Issues
Good hand hygiene and attention to food safety guidelines are practices important at home and even more so when traveling. Consider yourself fortunate if you’ve never had what’s commonly lumped together under the generalized term ‘food poisoning’. The risk for serious complications due to food borne illness increase for people with chronic diseases, who are either very young or elderly, who are pregnant, or who have impaired immune systems. Need a quick review of tips about ‘the good, the bad, and the ugly’ when it comes to food and drink safety? This resource from the U.S. CDC gives a nice overview in plain language, Food and Drink Considerations When Traveling.
Matters can move from ‘uncomfortable’ to ‘life-threatening’ when navigating a food-borne illness caused by eating or drinking food or water contaminated with certain types of Escherichia coli (E. coli) bacteria. That’s why it’s so important to reduce your risks. Certain types of E. coli are harmless and can normally maintain a presence in a healthy digestive tract. Other types of E. coli can cause diarrhea in what’s commonly known as ‘Traveler’s Tummy’ such as Enterotoxigenic Escherichia coli (ETEC) or Enteroaggregative Escherichia coli (EAEC) which are often found in food and water in areas with poor sanitation or in developing nations. Another harmful E. Coli strain is Enteroinvasive Escherichia coli (EIEC), which usually comes from eating contaminated vegetables, undercooked meat, or drinking unpasteurized (raw) milk. In addition to digestive tract issues, symptoms of EIEC can include vomiting, fever, chills, and blood or mucus in stools. Think about it – if fruits and vegetables aren’t washed before cutting, a knife can drag outer germs through fresh produce. Cooking can kill most, but not all, microorganisms which cause such illnesses.
One form called Shiga toxin-producing E. coli (STEC, sometimes known as STEC-HUS) can be life-threatening and requires immediate medical care. No, STEC-HUS isn’t atypical HUS but a different illness requiring different medical intervention and treatment. No, if you’re a patient being treated with eculizumab or ravulizumab you are not protected from becoming ill when infected with Shiga toxin-producing E. coli. (FMI on E.coli click HERE) Since STEC-HUS is more common than atypical HUS, most doctors will have seen other causes of food-borne infection, so if you’ve been diagnosed with aHUS do carry documents to verify your diagnosis. (Click HERE to view a brief video on STEC-HUS vs aHUS)
Learn how to decrease the risk of food borne illness to avoid the unpleasantness of traveler’s diarrhea and stomach cramps. Street food is appealing, but it’s difficult to gauge whether food prep utensils and serveware (e.g. cups, serving platters, utensils) have been properly handled/cleaned. Ingredients and menu items need to be stored and served at appropriate temperatures to avoid bacterial growth. Different knives and cutting boards need to be utilized, with different ones for raw meat versus separate ones for vegetables. That fancy drink might prove a risk if ice cubes aren’t made from a safe water supply or made with bottled water. Use of bottled water to brush teeth is a wise extra step. Peeled fruits and vegetables or those which are cooked are less apt to be contaminated than eating them raw or with ‘skin on’, but some contaminants are known to be transmitted through their thin skins or porous rinds. Sadly, if there’s any question of food safety standards when tempted to select a delicious fruit smoothie or green veggie drink, you may need a re-think in favor of another beverage selection or by choosing a bottled version which has been pasteurized. It’s not just E.coli bacteria either. Salmonella and Listeria also are among the pathogens which cause such illness, whether traveling or at home, to cause what’s commonly known ‘food poisoning’ (FMI on food safety click HERE).

Your Travel ‘First Aid Kit’
Nothing ruins a holiday more than feeling unwell, but if you’re traveling for work it’s pretty difficult to make a positive impact when health issues arise. Somehow, a busy day can distract from aches and pains, but when the evening rolls around it’s best to have some ‘just in case’ medications to ease symptoms. Don’t expect to see your nation’s popular ‘over the counter’ medication brands when traveling abroad. Do expect to spot OTC medications which may bring relief, but if you’re not a linguistic genius, plan on asking a friendly pharmacy staffer to translate drug package directions into your native language. Certain medications may not be ‘kidney friendly’, so check with your doctor for a list of cold medications, pain relievers, and other preparations that are right for you. Some nations sell common antibiotics without a prescription, and based on travel regions your travel medicine specialist may recommend certain vaccinations prior to your trip (such as for typhoid or malaria). Cholera remains a global threat and is a bacterial infection caused by eating or drinking food or water that is contaminated. Dysentery is an intestinal infection caused by bacteria or parasites, with symptoms that include vomiting and diarrhea (FMI on dysentery, click HERE). Typhoid, also called typhoid fever or enteric fever, is caused by water or food contaminated with a strain of salmonella bacteria. The World Health Organization recommends typhoid vaccines for residents or travelers to certain nations. Work together with your medical team, especially if you’re traveling abroad, since no vaccine is foolproof and even so there’s not a vaccine for every illness.
Prior to packing your suitcase, consider not only your regular medications but also what you might need if you’re feeling unwell. Make a checklist. Know that not all medications, such as CBD containing products and Schedule II controlled substance prescriptions for narcotics and stimulants, may be legally allowed in all states, regions or countries. Check with your medical providers to see if it’s advised that you bring antibiotics* (such as azithromycin or ciprofloxacin) on hand ‘just in case’ for certain global travel regions where stomach cramps and diarrhea might signal serious illness like an E.coli infection. Ask your doctor what symptoms might signal a serious medical illness, to help guide your decision on when to seek medical care during your trip. Consider packing ‘over the counter’ medicines that are dual purpose, like for GI issues that may appear in combination* (upset stomach,diarrhea, cramps, nausea). A good rule of thumb? If you’ve used a health product or OTC drug in the last half-year, consider whether it’s wise to bring it along in your Travel First Aid Kit… ‘just in case’.
Travelers: Be Prepared & Make Good Choices
Sometimes it’s important to go back to a very basic truth, having atypical HUS doesn’t define you or your life. You may need to plan ahead a bit more, and work within certain limitations depending on your travel locations. Look at options, check with your medical team, be flexible, plan thoroughly and in advance. Whether for work or pleasure, keep a positive attitude and plan for a successful trip.
**Note: As a global patient organization and non-profit advocacy group, we do not provide medical advice. The information in this overview is meant as a guide to launch discussion with your medical team, and cannot replace conversation with your physician(s) about your personal situation. As such we do not endorse or assume liability for material presented here.

