Most babies are born healthy. Even those susceptible to aHUS due to genetic abnormalities are born healthy. Although it is rare, it has been known for newborns to onset within weeks.Screening for certain conditions in all new born babies is now a routine practice in countries and states which have approved its use.
EURORDIS has produced a booklet about the principles underpinning new born screening , it can accessed HERE) , A simple heel prick for a blood sample is all that needs to be done and is usually taken a few days after birth. The blood is then analysed to determine any onset /susceptibility to a range of illnesses.
Most screening tests are negative and parents will hear no more about it. A positive test does necessarily mean the baby is ill and needs treatment , but it is likely the will in the future.
Could aHUS become one of those conditions for screening asks Lexi and Tre?

The following list gives the 35 conditions for screeing in Virginia, USA. It is a long list but aHUS is not one of them. Not all of these conditions get selected for screening by other States or Countries who have decided what is screened for in their own panels.
What conditions are Screened For in Virginia? (UPDATE check other states using this LINK to EveryLife Foundation for Rare Diseases Website)
Amino Acid Disorders
- Argininosuccinic Aciduria (ASA)
- Citrullinemia, Type I (CIT)
- Classic Phenylketonuria (PKU)
- Homocystinuria (HCY)
- Maple Syrup Urine Disease (MSUD)
- Tyrosinemia, Type I (TYR I)
Endocrine Disorders
Fatty Acid Oxidation Disorders
- Carnitine Uptake Defect (CUD)
- Long-Chain L-3 Hydroxyacyl-CoA Dehydrogenase Deficiency (LCHAD)
- Medium-Chain Acyl-CoA Dehydrogenase Deficiency (MCAD)
- Trifunctional Protein Deficiency (TFP)
- Very Long-Chain Acyl-CoA Dehydrogenase Deficiency (VLCAD)
Hemoglobin Disorders
- S, Beta-Thalassemia (Hb S/ßTh)
- S, C Disease (Hb S/C)
- Sickle Cell Anemia (Hb SS)
Lysosomal Storage Disorders
- Mucopolysaccharidosis Type-I (MPS I)
- Pompe (POMPE)
Organic Acid Conditions
- 3-Hydroxy-3-Methylglutaric Aciduria (HMG)
- 3-Methylcrotonyl-CoA Carboxylase Deficiency (3-MCC)
- Beta-Ketothiolase Deficiency (BKT)
- Glutaric Acidemia, Type I (GA-1)
- Holocarboxylase Synthetase Deficiency (MCD)
- Isovaleric Acidemia (IVA)
- Methylmalonic Acidemia (Cobalamin Disorders) (Cbl A,B)
- Methylmalonic Acidemia (Methymalonyl-CoA Mutase Deficiency) (MUT)
- Propionic Acidemia (PROP)
Other Disorders
- Adrenoleukodystrophy (ALD)
- Biotinidase Deficiency (BIOT)
- Classic Galactosemia (GALT)
- Critical Congenital Heart Disease (CCHD)
- Cystic Fibrosis (CF)
- Hearing loss (HEAR)
- Severe Combined Immunodeficiency (SCID)
- Spinal Muscular Atrophy (SMA)
Few will be familiar with many of them. Probably the best known being sickle cell disease and cystic fibrosis. Both those two diseases are rare but are more common than aHUS. Sickle cell much more so, but it shares Complement as a disease mechanism.
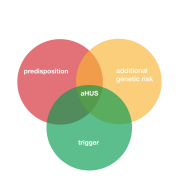
Being predisposed to aHUS does not mean that someone will onset. Ever. If screening led to treatment it would mean that some people would have preventative treatment for life, unnecessarily. Most of the few who will onset do not onset with aHUS until they are 30 years old, or more, so for many treatment would be wasted.
Those who have no known genetic variant would not test positive of course. So such screening would not be fully inclusive for around 40% of potential aHUS patients. Some who have a family history of aHUS would not likely be surprised if a new born was susceptible.
But knowing about having a predisposition to aHUS is of interest for many, but not always to all of those susceptible. Even if they never need treatment.
Like other States Virginia has a Committee to decide which diseses should be screened for. At this link the process is illustrated in the way the decision on whether to include Krabbe’s Disease was made. ( HERE).
Of specific interest in the account , are the reasons given for a decision not to include Krabbe Disease on the panel for screening:
1. Krabbe Disease is not one of the disorders on the RUSP. Disorders on the RUSP are chosen
based on evidence that supports the potential net benefit of screening, the ability of states to
screen for the disorder, and the availability of effective treatments. Krabbe Disease was
reviewed for consideration to be added to the RUSP in 2009 and not approved;
2. The lack of data on the number of EIKD cases exclusively identified through NBS without any
family history or prenatal diagnosis;
3. The inability for identified infants to receive care within Virginia due to the lack of an available
pediatric transplant center. Concerns of receiving treatment within a narrow window with
documented cases of delays in receiving care outside of the state and inequality for the Virginia
Medicaid population;
4. The potential for a high rate of intermediate or borderline results (PSY of 2-10) and lack of
genotype/phenotype correlation will lead to significant psychological distress and a medical
odyssey for families in attempting to confirm or refute the diagnosis.
aHUS would fail at the first hurdle as it it not one of the diseases the Federal Government’s Recommended Uniform Screening Panel ( RUSP) .
It is unlikely too that there is any data on aHUS incidence or prevalence in Virginia. Estimates would be for the State’s 8 million population would be 4 aHUS cases per year and 40 surviving patients, but no one really knows. It is unlikely there is a centre of excellence dedicated to aHUS in Virginia. And finally not all results of genetic tests are conclusive nor always predictive of disease onset.
It is very unlikely therefore that aHUS would be added to the panel in Virginia alone. But you have certainly brought this issue to the attention of the aHUS Community, Lexi and Tre. An issue that is going to develop into something much bigger. Something which is becoming of international interest . Genetic testing is becoming cheaper and easier. The subsequent counselling needed would probably be more of a challenge.
If there was a national interest for aHUS screening in the USA .the starting place would be the Federal Department of Health. Who would lead on that is another question? The process for doing so is likely to be of common interest to all Rare Disease organisations.
Here is an extract from the UK’s Rare Disease Plan relating to screening of newborns and the research planned on whole genome screening of 100,000 newborn babies to make better decisions about the value of disease screening inclusion.
“Action 2: Whole Genome Sequencing (WGS) to screen for genetic conditions in healthy newborns
Scientific advances mean that there are an increasing number of conditions where interventions are available to reduce or avoid harm, or improve long-term outcomes, if the condition is detected early. WGS could significantly increase the diagnoses of genetic conditions not currently covered by the NHS newborn blood spot screening programme.
Guided by the outputs of the public dialogue on WGS in newborns published in July 2021, Genomics England and NHSE/I are leading a programme to explore the benefits, risks and broader implications of WGS in newborns.
This includes co-designing and running an ethically approved research pilot using WGS to screen for rare genetic conditions in healthy newborns. New funding for this research pilot was announced in the October 2021 Spending Review. The research pilot will:
- sequence the genomes of up to 100,000 newborns and follow their progress to better understand the clinical benefits and potential risks of newborn genomic screening, aiming to accelerate diagnoses and access to treatments for rare genetic conditions
- be designed through careful consultation with the rare disease community, healthcare professionals, the UK National Screening Committee and other key stakeholders – for instance, through their NHS Steering Group
- include careful testing of how the whole pathway – from diagnosis through to genetic counselling and care – can be rolled out within the NHS, if there is proven benefit
- ensure robust processes are in place for consent, return of results, data use and access
- develop a framework to identify genes for targeted analysis, based on clinical and genomic evidence and wide consultation. Outputs from the consultation to date have led towards a focus on diseases that present in early childhood for the research pilot, where an outcome-changing action would be available if they were detected earlier
- improve understanding of the patient experience of genomic newborn screening
- provide evidence to support the UK National Screening Committe to make recommendations for future NHS screening programmes“
This is a subject that will stay and develop over the next decade. aHUS patients and families views on genetic testing should drive what happens for our diseases. It might require a special research project at some time, Lexi and Tre.
Article No. 506