Article No 389
27 October 2020
A process is a series of steps. Diagnosis is a process. A medical diagnosis is the process by which a persons symptoms and signs are explained by a disease or a condition. aHUS has symptoms and signs and the challenge is for them to be recognised by clinicians as aHUS.
Clinical signs which define aHUS include the “triad” of haemolytic anaemia, thrombocytopenia and uraemia. These signs are not visible to the patient and are only visible in tests of the patient’s blood. Without those tests what aHUS is doing cannot be seen.
But even as these manifestations are bubbling under the patient might notice symptoms which stem from them. The patient might feel tired and easily exhausted because of falling red blood cells caused by the anaemia. The patient might feel nauseous or have traces of blood in their urine because their kidneys are failing. Low blood platelets caused by the thrombocytopenia may not be visible to the patient, unless they cut themselves and the bleeding does not stop. So on the surface something is going on which may produce signs which are common to a number of illnesses.
It is not unusual for an aHUS patient to regard themselves in the peak of health, the fittest they have ever been before their illness. Even when something has already triggered and which is going to make them seriously ill. These are the first two steps in the process towards a diagnosis of aHUS.
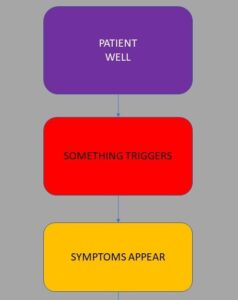
The third step is when symptoms appear, some of which are mentioned earlier, and like everyone does the patient might explain them away as something common and that they are aware of, e.g. a cold or flu , a stomach bug and treat them as such. They may even undertake self clinical testing by taking their temperature. The symptoms may also be down to the triggering condition , just to confound matters.

Meanwhile the unseen smoldering clinical problems develop, and the symptoms get a bit more severe or show no sign of improving. At which point the patient would seeks medical advice. Thus begins an important journey through the health care provider steps to get a diagnosis which explains what is wrong with them.
This journey is rarely a step by step linear process and is more likely to be iterative process which results in patients returning to previous steps, or within one step stuck short of a diagnosis There may be uncertainty or misdiagnosis because the symptoms could be shared with other diseases, or because the clinician may not be aware of the ultra rare disease aHUS.
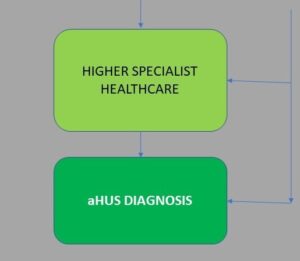
The process steps may include healthcare providers in tiers of general or specialist practice. It may involve a range of different specialists and different tests.
As always when “mapping” any process there are the exceptions – the “ah buts”. In this case its “Ah but what about those who are already receiving specialist care when aHUS triggers. Their trigger might be caused by a transplant or pregnancy or even another condition they have that leads to uncontrolled Complement”. Good point but it just might give them a head start in the process as their entry starts at the specialist healthcare level where there might be an elevated awareness of aHUS. But there may be other explanations of what is happening to the patient.
Suspicion and thinking of aHUS is more likely during specialist or higher specialist healthcare steps Those providers through observing symptoms, measuring signs, undertaking their tests including by then maybe a kidney biopsy, are able to disentangle it all to arrive at atypical Haemolytric Uraemic Syndrome as the cause of the patients state of health. “You’ve got aHUS”. The aHUS Diagnosis Process end point
What caused it and how it is treated determines what happens next and the outcome (prognosis). What follows is in the post diagnosis management of aHUS process.
But to get to that process the aHUS diagnosis is pivotal. Each patient will have faced both similar and different experiences in getting their diagnosis. Things will have happened to speed up and to slowdown getting there. All of which will influence their individual timelines from being well to being told they have aHUS. That timeline can determines outcome too.
aHUS patients ask the question in their Global aHUS Research Agenda:
“Is there a diagnosis sweet spot which can be found before a developing thrombotic microangiopathy turns into a catastrophic episode of aHUS?”
This question is born of the experience of them going through the aHUS diagnosis process, and, with hindsight, wondering whether their diagnosis could have been made earlier with better outcomes. An earlier diagnosis to reduce both their physical and mental injury during the worst of their onset.
That “sweet spot” might be elusive and different for all. It comes after anaemia and kidney problems are evident. and when the tests reveal the “triad”.
aHUS patients know how the identification of a thrombotic microangiopathy, or TMA, is key to their diagnosis. They also know that TMAs come in many shapes and forms, and aHUS is but a very minor sub group among them all.
So an aHUS diagnosis must overcome there being a constellation of symptoms, which each patient may ,or may not, have, and a disease which clinicians may, or may not, be aware of in hope that someone can eventually join the dots to reveal aHUS.

A complete version of the aHUS Diagnosis Process Flow Chart can be seen here Flowchart
Previous articles on aHUS diagnosis by aHUS Global Action:
AHUS DIAGNOSIS: TIME IS OF THE ESSENCE
THE AHUS DIAGNOSIS CHALLENGE
FINDING A NEW NORMAL AFTER DIAGNOSIS
AHUS DIAGNOSIS & TREATMENT – KDIGO CONTROVERSY CONFERENCE
WHERE WE ARE UP TO ON AHUS DIAGNOSIS AND TREATMENT
IS IT AHUS? PERHAPS IT’S TTP, STEC-HUS, OR ANOTHER TMA
AHUS PATIENT CARE – THE NEED FOR MULTIDISCIPLINARY COLLABORATION

