All aHUS patients know that when on complement inhibitor treatment they are at risk of meningococcal infection.
Do they?
Of course, they are told about it before they get treatment.
Do they?
Yes their clinician tells them. They tell them about the risk and about the symptoms to recognise its onset if they do become infected.
But no one gets infection do they? It’s so rare.
The bug is really quite common, its name is so fancy it is written in Latin/Greek and italics neisseria meningitidiss. About 10% of people have it up their nose but will never be ill from it, they just carry it. Those who do become ill, they are said to have illnesses due to meningococcal infection.
Illnesses?
Yes the infection can lead to serious illnesses, a couple of them like meningitis ( full name meningococcal meningitis) or septicemia (fancy name “meningococcemia”) are the best known. Both are serious and life threatening.
How life threatening?
Very, and they can rapidly appear and cause death in hours.
That is scary.
Indeed and that has happened to people on complement inhibitors in past.
What sort of numbers are we talking about here ?
Not much information about it but one report four or five years ago found about 3 patients per 1000 patients on a complement inhibitor will get an infection each year and 1 of those every three years could die.
Wow there are thousands of patients on complement inhibitors for aHUS , PNH etc these days.
Absolutely though we do not how many thousands. Nor do we know where in the world aHUS patients are getting infected. But the CDC provides some information for the USA.
CDC?
Yes the Centre for Disease Control and Prevention. Infectious diseases like meningococcal have to be reported to the CDC whenever they happen. The CDC has data and make it public.
Including information about those on Complement Inhibitors?
Yes it is one of the group that CDC has a special interest in. Just look at this information extracted from the CDC’s website.
| YEAR | TOTAL CASES | Complement Inhibitor | College Students | Homeless | Men to Men Sex |
| 2020 | 235 | 4 | 10 | 14 | 1 |
| 2019 | 375 | 5 | 21 | 9 | 10 |
| 2018 | 329 | 4 | 18 | 16 | 5 |
| 2017 | 350 | 0 | 39 | 9 | 18 |
| 2016 | 372 | NR | 32 | NR | 31 |
| 2015 | 358 | NR | 23 | NR | 15 |
I am not good with figures but if I understand it right total annual meningococcal infection cases are pretty much the same until COVID year 2020. Complement inhibitor figures started to feature from 2017, along with the homeless data. There are 4 to 5 cases complement inhibitor meningococcal reported per year it is the lowest of the groups which are specially reported.
That is right and their number did not drop like others did in 2020. Also infection numbers remain almost the same even though by 2020 more patients would be getting treatment than in 2017.
But why if numbers are so much lower is CDC interested in complement inhibitor linked meningococcal infection?
Think about the number of people living with other life styles they would run into the high hundreds of thousands or several millions. Their infections might be higher but the likelihood of getting an infection is considerably less. In the USA’s general population of about 330 million the chances of being one of 350 or so people to get an infection is around a million to one. Your chances of an infection in a US college student population of 19 million is about 750,000 to 1. There may only be 4000 to 8000 people on complement inhibitors in the USA so they face odds of just 1000 to 2000 to 1. It is much more likely to happen to them than anyone else. That is why the CDC is interested .That is why it does so much to raise awareness of aHUS patients’ risk of having a meningococcal infection. See what they say about managing this risk on its website HERE.
Woah I have just read their first two sentences “Recent data suggest that meningococcal vaccines are likely provide incomplete protection against invasive meningococcal disease in people receiving eculizumab. Experts believe this increased risk likely also applies to people receiving ravulizumab . Vaccinations do not always work!?
Yes generally vaccinations do not always work, just look at the noise in the media about the COVID vaccinations and their pros and cons.
But let’s focus on ourselves.
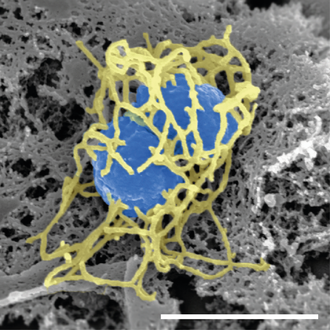
OK sorry , we know that Complement is the first responder of the innate immune system to join the hunt for invading bacteria like neisseria meningitidiss (see image). When it finds it, Complement’s membrane attack complex penetrates it and its innards spill out. Not a pretty sight, but it is destroyed. If Complement is inhibited then it cannot do that ,neisseria meningitidiss has free rein, so additional defences are needed. That is what the vaccination gives. It provides the person with a safe meningococcal like “infection” so another part of the immune system can create antibody which can destroy the actual bacteria. Except…
Except?
Yes except. It takes time for the vaccination to be effective. About two weeks or so. That is why those newly treated with a complement inhibitor are given antibiotics to give them some interim protection waiting for the vaccination to kick in. Some patients will continue to take them for as long as they are on treatment because they add protection from meningococcal infection. Patient’s clinicians may have different ideas about whether to do that or not. Whatever they do, they should at least explain it to the patient.
But also there are several types of bacteria , each identified by a letter and the current vaccinations available are only effective against those lettered ACWY and B. It is a condition of use that all complement inhibitor treated patient are vaccinated but not all get the vaccination for bacteria B. ACWY and B are the most common types of neisseria meningitidiss.
Also the antibodies resulting from the vaccinations have a limited life span and in time they disappear and a booster vaccination is needed. There is a lot of confusion about when a booster be given and whether the levels of antibodies are being monitored sufficiently. If their last vaccination was three years or more ago patients should at least be asking their doctor to measure their antibodies and get a booster vaccination if they are too low for protection.
Gosh that is a lot to think about. But it is all the responsibility of the patient’s clinicians. They know about these things
They should, but, as we have seen with boosters , the patient has to play a part too. Patients are responsible for themselves too. They must be alert to the risk and vigilant to the possibly of it striking them. Vigilant but still live their lives as full as possible , not being too obsessive and nor being in a reckless denial.
?So that if does happen they will be the first to know and react, and react quickly.
How will they know?
They will feel unwell and show some symptoms. They will not know for certain that it is a meningococcal infection but they should seek medical attention rapidly. To get clinicians’ attention patients may have to play the patient safety card which all patients have been given for such circumstances . Clinicians can then do tests to confirm a diagnosis or not and start treatment. Targeted antibiotics can work. Even if it is not meningococcal infection patients have done the right thing, it is not a case of crying “wolf”.
How will they know the symptoms to watch for?
They will have seen them in the information leaflet for patients that comes with every vial package of eculizumab and ravulizumab. Haven’t they? ( If not ask for a copy on your next infusion, it could answer more questions you have about these drugs). They are also listed on the patient safety card which can be a quick “aide memoire” as patients always keep those cards to hand. Don’t they ( If you have lost yours or it has disintegrated with age or been chewed by the dog ask for a new one).
Could you not tell us the symptoms?
OK I will tell you what the CDC says and they have pictures of them too:
The most common symptoms for MENINGITIS include:
- Fever
- Headache
- Stiff neck
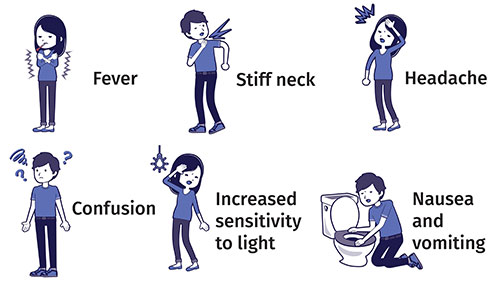
There are often additional symptoms, such as
- Nausea
- Vomiting
- Photophobia (eyes being more sensitive to light)
- Altered mental status (confusion)
And SEPTICEMIA
- Fever and chills
- Fatigue (feeling tired)
- Vomiting
- Cold hands and feet
- Severe aches or pain in the muscles, joints, chest, or abdomen (belly)
- Rapid breathing
- Diarrhea
- In the later stages, a dark purple rash
Thanks I get the idea. They are both meningococcal infections but their symptoms only overlap a little. Any other advice?
Only behavioural, not clinical not allowed to do that. Lifestyle has a lot to do with being exposed to infection. Also aHUS patients should be alert to news about any outbreaks of infection in their locality. You would be very unlucky to do so but it is possible to have meningococcal infection more that once, so vigilance is still needed even after surviving an infection.
Surviving ?
Yes people more often than not do survive. People in the general population will not be as alert as those on a complement inhibitor, they will rarely be vaccinated. They are more likely to delay going to a doctor and that will lead to more serious consequences.
So risk knowledge, awareness of symptoms , vaccinations, antibiotics, alertness and swift patient action saves the day.
Yes in a nutshell. Pass that on.
Article No. 571
Previous article

Some side effect- Meningococcal infection!
The side effects of treatment and residual ailments of an aHUS onset featured highly by aHUS families in the contribution to the aHUS Patients Research Agenda. The topic is covered…

